Non Alcoholic Fatty Liver
Non-Alcoholic Fatty Liver Disease (NAFLD)
Overview
Non-alcoholic fatty liver disease (NAFLD) is an umbrella term for a range of liver conditions affecting people who drink little to no alcohol.
The main feature of NAFLD is the excess buildup of fat in the liver cells, which can lead to liver inflammation and damage over time.
Symptoms
Many people with NAFLD may have no symptoms, especially in the early stages. When symptoms appear, they may include:
-
Enlarged liver
-
Fatigue
-
Pain or discomfort in the upper right abdomen
-
Abdominal swelling (ascites)
-
Enlarged blood vessels just beneath the skin's surface
-
Enlarged breasts in men (gynecomastia)
-
Enlarged spleen
-
Red palms
-
Yellowing of the skin and eyes (jaundice)
Effects (Complications)
If left untreated, NAFLD can progress and cause:
-
Liver inflammation (non-alcoholic steatohepatitis, or NASH)
-
Fibrosis (scarring of liver tissue)
-
Cirrhosis – severe scarring that affects liver function
-
Liver failure in advanced cases
-
Increased risk of liver cancer
-
Metabolic complications such as type 2 diabetes, obesity, high blood pressure, and heart disease
Treatment
There is no specific medication for NAFLD yet. Treatment mainly focuses on lifestyle changes and managing related conditions:
Lifestyle & Medical Care
-
Weight loss – losing 7–10% of body weight can reduce fat in the liver
-
Healthy diet – a balanced diet rich in fruits, vegetables, whole grains, and lean protein; avoid sugary drinks and processed foods
-
Regular exercise – at least 30 minutes of physical activity most days of the week
-
Control diabetes, blood pressure, and cholesterol – with medicines if necessary
-
Avoid alcohol – even small amounts can worsen liver damage
-
Medications – Vitamin E or insulin-sensitizing drugs (like pioglitazone) may be recommended in select cases under medical supervision
Homeopathic Support (Complementary Care)
(Helps improve liver function and reduce symptoms; must be guided by a qualified homeopath)
-
Chelidonium majus – for liver pain and jaundice
-
Lycopodium – for bloating, digestive issues, and liver weakness
-
Carduus marianus – supports liver detox and reduces fatty deposits
-
Nux vomica – for liver damage linked to poor digestion or lifestyle stress
-
Phosphorus – for fatigue and weakness due to liver dysfunction
Note: Early detection and lifestyle modification are the key to preventing progression from fatty liver to cirrhosis or liver failure.
Primary Biliary Cholangitis
Primary Biliary Cholangitis (PBC)
Overview
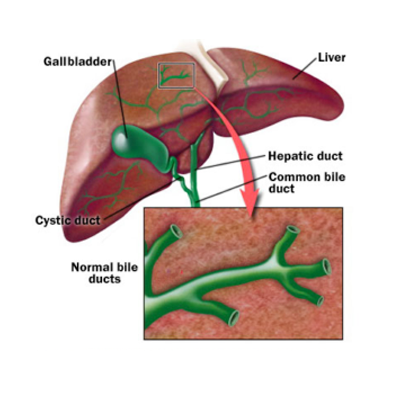
Primary biliary cholangitis (PBC), previously called primary biliary cirrhosis, is a chronic liver disease in which the bile ducts in the liver are gradually destroyed.
Bile is a digestive fluid produced by the liver that helps absorb fats, vitamins, and remove toxins and worn-out red blood cells. When bile ducts are damaged, bile can accumulate in the liver, causing inflammation and irreversible scarring (cirrhosis) over time.
PBC progresses slowly and is more common in middle-aged women, though it can affect anyone. Early detection and treatment can slow disease progression and manage symptoms.
Symptoms
Early symptoms of PBC may include:
-
Fatigue
-
Itchy skin (pruritus)
-
Dry eyes and mouth
-
Pain in the upper right abdomen
-
Swelling of the spleen (splenomegaly)
-
Muscle, bone, or joint pain
-
Swollen feet and ankles (edema)
As the disease progresses, additional signs may appear:
-
Jaundice (yellowing of the skin and eyes)
-
Dark urine and pale stools
-
Easy bruising or bleeding
-
Osteoporosis due to poor vitamin absorption
Effects
-
Chronic liver inflammation leading to scarring and cirrhosis
-
Liver failure in advanced stages
-
Portal hypertension causing swelling in the legs and abdomen
-
Fatigue and reduced quality of life
-
Complications in other organs, such as bones (osteoporosis)
Treatment
1. Medications:
-
Ursodeoxycholic acid (UDCA) to slow liver damage and improve bile flow
-
Obeticholic acid for patients who do not respond to UDCA
-
Antihistamines or cholestyramine for itching
-
Vitamin supplements (A, D, E, K) to address deficiencies
2. Lifestyle and Supportive Care:
-
Healthy diet to reduce liver stress
-
Regular exercise to maintain muscle and bone strength
-
Avoid alcohol and hepatotoxic medications
3. Advanced Treatments:
-
Liver transplant for end-stage disease or liver failure
Hepatotoxicity
Overview
Toxic liver disease refers to damage to the liver caused by harmful substances. It is also called hepatotoxicity or toxic hepatitis. Without timely treatment, this condition can result in serious health problems.
The severity can vary—some cases are mild, while others progress to permanent liver scarring (cirrhosis). Advanced damage may cause liver failure and can even be life-threatening. In certain cases, such as with an overdose or even short-term use of drugs like acetaminophen (paracetamol), liver failure may occur rapidly.
Symptoms of Hepatotoxicity
Possible signs and symptoms include:
-
Rash on the skin
-
Abdominal or stomach pain
-
Nausea and vomiting
-
Persistent fatigue or weakness
-
Dark-colored urine
-
Pale or clay-colored stools
-
Yellowing of the skin and eyes (jaundice)
-
Loss of appetite
-
Fever

Gallstone-
Gallstones – Overview (Spaks Homeopathy)
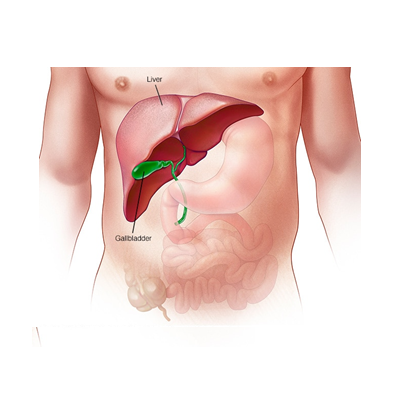
Gallstones are hardened deposits of digestive fluid (bile) that form inside the gallbladder. The gallbladder is a small, pear-shaped organ located beneath the liver, responsible for storing and releasing bile into the small intestine to aid digestion.
Gallstones can vary in size, ranging from a tiny grain of sand to as large as a golf ball. Some people may develop only a single gallstone, while others can develop multiple stones at the same time. While many gallstones are silent and cause no symptoms, they may also lead to severe abdominal pain and complications when they block bile ducts.
Causes of Gallstones
-
Imbalance in the substances that form bile (cholesterol, bile salts, bilirubin)
-
Excess cholesterol in bile leading to crystallization
-
Poor gallbladder emptying causing bile stasis
-
Obesity or rapid weight loss
-
Family history of gallstones
-
Female gender, pregnancy, and hormonal changes (estrogen influence)
Symptoms of Gallstones
-
Severe, sudden pain in the upper right abdomen (gallbladder colic), sometimes radiating to the upper back or right shoulder
-
Nausea and vomiting
-
Fever with chills (if infection develops)
-
Jaundice (yellowing of skin and eyes due to blocked bile flow)
-
Clay-colored stools or dark urine
-
Indigestion, bloating, or discomfort after fatty meals
Effects / Complications
-
Acute gallbladder inflammation (cholecystitis)
-
Blockage of bile ducts leading to severe pain and infection
-
Pancreatitis (if gallstones block the pancreatic duct)
-
Chronic digestive issues
-
Increased risk of gallbladder cancer (rare but serious)
Homeopathic Treatment for Gallstones (Spaks Homeopathy)
Homeopathy helps in managing gallstone-related pain, improving bile flow, and reducing the tendency to form stones. Some commonly used remedies include:
-
Chelidonium Majus – for right-sided abdominal pain radiating to the back and shoulder
-
Lycopodium Clavatum – for bloating, nausea, and gallstone colic, worse in the evening
-
Carduus Marianus – for gallbladder and liver disorders with jaundice
-
Calcarea Carbonica – for individuals prone to gallstone formation with sluggish digestion
-
China (Cinchona Officinalis) – for weakness, gas, and bloating after gallstone attacks
Note: Remedies must be chosen according to individual symptoms. Consultation with a qualified homeopathic physician is recommended for safe and effective treatment.
.jpg)