Mastoiditis
Overview
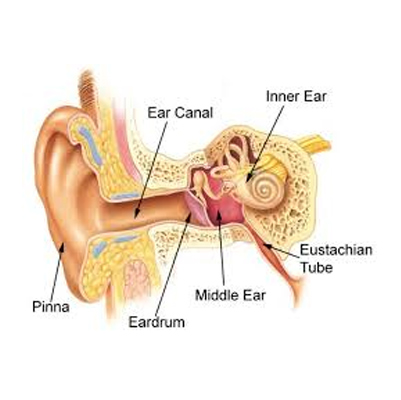
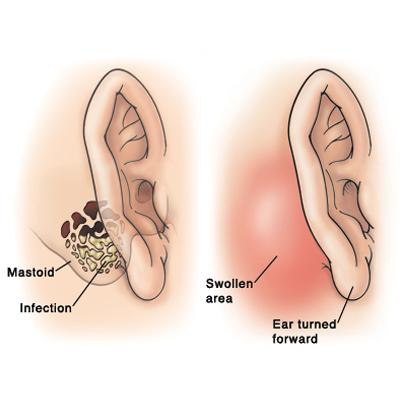
Mastoiditis is a bacterial infection of the mastoid air cells, located in the temporal bone behind the ear. These air cells help regulate ear pressure, protect delicate ear structures, and may cushion the bone during trauma.
Mastoiditis usually develops as a complication of an untreated or severe middle ear infection (otitis media). Because the mastoid bone is close to the brain and other vital structures, infection can spread beyond the mastoid and lead to serious, potentially life-threatening complications if not treated promptly.
Symptoms
-
Fever, irritability, and lethargy
-
Swelling of the earlobe
-
Redness and tenderness behind the ear
-
Drainage (pus or fluid) from the ear
-
Bulging or drooping of the ear
-
Hearing loss (in some cases)
Effects (If Untreated)
-
Spread of infection to surrounding tissues
-
Formation of a mastoid abscess
-
Meningitis (infection of the brain’s protective layers)
-
Brain abscess
-
Facial nerve paralysis
-
Permanent hearing loss
Treatment
Medical Treatment
-
Antibiotics (IV or oral) to clear infection
-
Myringotomy (draining middle ear fluid via a small cut in the eardrum)
-
Surgery (mastoidectomy) if antibiotics fail or if abscess develops
-
Pain relievers and fever reducers
Home Care Support
-
Warm compresses behind the ear for comfort
-
Adequate hydration and rest
-
Strict follow-up with an ENT specialist
Homeopathic Support (Complementary, not a substitute)
-
Belladonna – for throbbing ear pain with redness and fever
-
Hepar sulphuris – when there is pus or ear discharge
-
Pulsatilla – for ear pain with thick yellow-green discharge, worse at night
-
Silicea – for chronic or recurrent ear infections with discharge
Meniere's
Meniere’s Disease
Overview
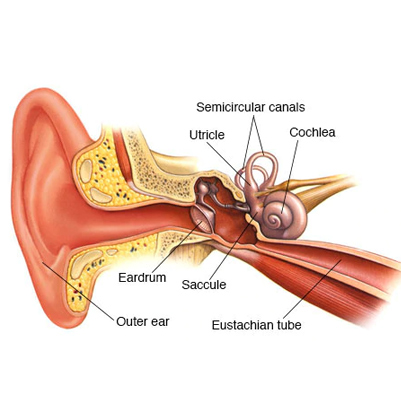
Meniere’s disease is a disorder of the inner ear that affects balance and hearing. It causes:
-
Episodes of vertigo (spinning sensation)
-
Tinnitus (ringing or buzzing in the ear)
-
Hearing loss
-
A feeling of fullness or pressure in the ear
It usually affects one ear. The attacks may come on suddenly or after a short period of muffled hearing or ringing. Some people experience rare, isolated attacks, while others may have several episodes close together over a few days.
In severe cases, people may lose balance suddenly and fall without warning. These episodes are called drop attacks.
Symptoms
-
Repeated episodes of vertigo (dizziness with spinning sensation)
-
Vertigo lasting 20 minutes to several hours (but less than 24 hours)
-
Severe dizziness causing nausea or vomiting
-
Hearing loss (may come and go early but can become permanent over time)
-
Tinnitus – ringing, buzzing, roaring, or hissing sound in the ear
-
Fullness or pressure in the affected ear
Effects / Complications
If untreated or progressive, Meniere’s disease may cause:
-
Permanent hearing loss in the affected ear
-
Frequent vertigo attacks leading to imbalance and falls
-
Drop attacks (sudden falls without warning)
-
Emotional stress, anxiety, and depression due to unpredictable attacks
-
Reduced quality of life from ongoing dizziness and hearing problems
Treatment
Medical / General Treatment
-
Dietary changes (low-salt diet, avoid caffeine and alcohol)
-
Diuretics (to reduce inner ear fluid buildup)
-
Vestibular suppressants (meclizine, diazepam) during vertigo attacks
-
Anti-nausea medicines (promethazine)
-
Hearing aids for permanent hearing loss
-
In severe cases: injections or surgery (for persistent vertigo not controlled by medicines)
Homeopathic Supportive Remedies (to be used under guidance of a qualified homeopath)
-
Cocculus indicus – for vertigo with nausea and weakness
-
Gelsemium – for dizziness with heaviness and trembling
-
Conium maculatum – for vertigo worsened by turning the head or lying down
-
China (Cinchona officinalis) – for tinnitus with sensitivity to sound
-
Phosphorus – for progressive hearing loss with ringing in the ears
This structure covers Overview → Symptoms → Effects → Treatment (Modern + Homeopathy) in simple and clear English.
Otitis Externa
Overview
An outer ear infection is an infection of the outer opening of the ear and the external auditory canal, which connects the visible part of the ear to the eardrum.
This condition is medically known as otitis externa, and the most common form is often called “swimmer’s ear”, since it frequently develops after swimming when water remains in the ear canal, creating a moist environment for bacteria or fungi to grow.
Symptoms of Otitis Externa
-
Swelling of the ear canal
-
Redness and warmth in or around the outer ear
-
Pain or discomfort (often worse when pulling the ear)
-
Discharge of pus or fluid from the ear
-
Itching in the ear canal
-
Excessive fluid drainage
-
Muffled or reduced hearing (due to swelling or blockage)
Effects
-
Can cause temporary hearing loss if the canal becomes blocked
-
Recurrent infections may lead to chronic otitis externa with persistent itching and discharge
-
Severe, untreated infections can spread to nearby tissues, causing cellulitis or, in rare cases, dangerous complications in people with weakened immunity (e.g., malignant otitis externa)
-
Pain and discomfort may interfere with sleep and daily activities
Treatment
1. Self-care and Relief
-
Keep the ear clean and dry
-
Avoid swimming until the infection heals
-
Do not insert cotton swabs or objects into the ear canal
2. Medical Treatments
-
Antibiotic or antifungal ear drops to fight infection
-
Steroid ear drops to reduce swelling and itching
-
Pain relievers (acetaminophen, ibuprofen) for discomfort
-
In cases of blockage, a doctor may gently clean the ear canal before applying treatment
3. Prevention
-
Dry ears thoroughly after swimming or bathing (tilt head, use a towel, or gentle warm air)
-
Use earplugs while swimming if prone to infections
-
Avoid inserting sharp objects or swabs into the ear canal
-
Maintain ear hygiene but without over-cleaning, since removing too much wax increases risk of infection

Otitis
Overview
An ear infection (acute otitis media) is usually caused by a bacterial or viral infection that affects the middle ear — the air-filled space behind the eardrum that contains the tiny vibrating bones (ossicles) of the ear.
Ear infections are much more common in children than adults, largely due to the structure of their Eustachian tubes and developing immune systems. They often cause pain, discomfort, and fluid buildup in the middle ear, which can interfere with hearing.
Symptoms of Acute Otitis Media
In infants and children, symptoms may include:
-
Persistent crying or irritability
-
Restlessness or sleeplessness
-
Pulling or tugging at the ears
-
Ear pain (otalgia)
-
Headache
-
Feeling of fullness or pressure in the ear
-
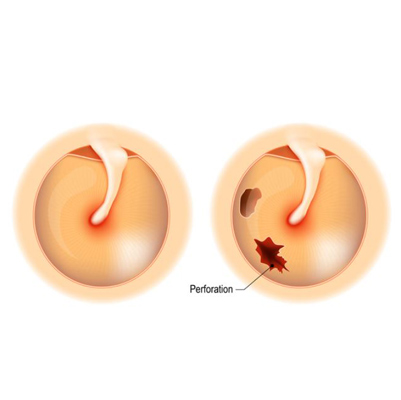
Fluid drainage from the ear (if the eardrum ruptures)
-
Temporary hearing loss
In adults, symptoms may also include:
-
Sharp or throbbing ear pain
-
Difficulty hearing
-
Dizziness or imbalance
-
Fever (sometimes present)
Effects
-
Recurrent ear infections can lead to hearing problems, which may affect speech and language development in children.
-
If untreated, infection may spread to nearby tissues, leading to complications like mastoiditis (infection of the mastoid bone) or, rarely, meningitis.
-
Repeated infections can cause perforation or scarring of the eardrum, leading to long-term hearing difficulties.
-
In adults, chronic infections may contribute to balance disorders and reduced quality of life.
Treatment
Treatment depends on the severity, age of the patient, and whether the infection is viral or bacterial:
1. Home Care & Symptom Relief
-
Warm compresses for pain relief
-
Adequate rest and fluids
-
Over-the-counter pain relievers (acetaminophen or ibuprofen)
2. Medical Treatments
-
Antibiotics (such as amoxicillin) if the infection is bacterial and severe, or if symptoms persist
-
Ear drops to relieve pain or inflammation
-
Decongestants or antihistamines (in select cases) to reduce Eustachian tube blockage
3. Surgical Options (for recurrent or chronic infections)
-
Myringotomy: A small incision in the eardrum to drain fluid
-
Tympanostomy tubes (ear tubes): Inserted to prevent fluid buildup and recurrent infections
4. Prevention
-
Vaccinations (flu and pneumococcal vaccines can reduce risk)
-
Breastfeeding infants (helps build stronger immunity)
-
Avoiding exposure to secondhand smoke
-
Practicing good hygiene to reduce upper respiratory infections
Otosclerosis
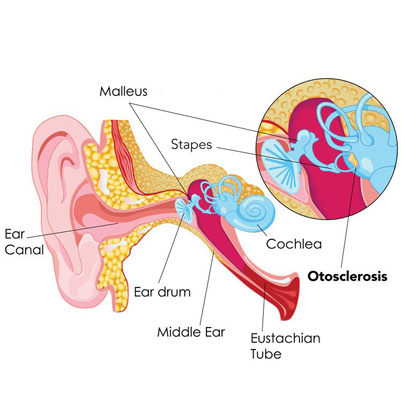
Overview
Otosclerosis is a rare condition that causes progressive hearing loss. It occurs when one of the tiny bones in the middle ear — most often the stapes (stirrup bone) — becomes fixed in place and cannot vibrate normally.
For proper hearing, sound waves must travel through the ear canal, vibrate the middle ear bones, and then reach the inner ear. When the stapes bone is stuck, sound cannot efficiently pass to the inner ear, resulting in hearing difficulties.
The condition usually develops gradually and may start with difficulty hearing low-pitched sounds or whispers. Over time, the hearing loss often worsens. Most people develop hearing impairment in both ears, though about 10–15% are affected in only one ear.
Symptoms of Otosclerosis
-
Gradual hearing loss (especially low-pitched sounds or whispers)
-
Speaking softly (due to reduced perception of own voice)
-
Hearing better in noisy environments (paracusis, a typical otosclerosis feature)
-
Tinnitus (hearing ringing, buzzing, or roaring sounds in the ear)
-
Hearing internal body sounds more loudly (e.g., chewing, breathing)
-
Dizziness or balance problems (in some cases)
Effects
-
Progressive hearing impairment that may eventually require hearing aids or surgery
-
Communication difficulties, leading to social withdrawal or reduced quality of life
-
Emotional stress such as frustration, anxiety, or depression due to hearing challenges
-
In severe cases, untreated otosclerosis can lead to significant hearing disability
Treatment
While there is no cure to reverse otosclerosis naturally, several treatment options can manage symptoms and restore hearing:
1. Hearing Aids
-
Amplify sound and are effective in mild to moderate cases.
2. Medications
-
In some cases, fluoride, calcium, or vitamin D supplements may slow disease progression, though evidence is limited.
3. Surgical Options
-
Stapedectomy: Removal of the immobile stapes bone and replacement with a prosthetic device to restore sound transmission.
-
Stapedotomy: A small hole is made in the stapes footplate, and a prosthesis is inserted — a less invasive variation.
4. Supportive Measures
-
Regular hearing tests to monitor progression
-
Counseling or support groups to help cope with emotional effects
-
Communication strategies (lip-reading, assistive listening devices)
Ramsay Hunt syndrome
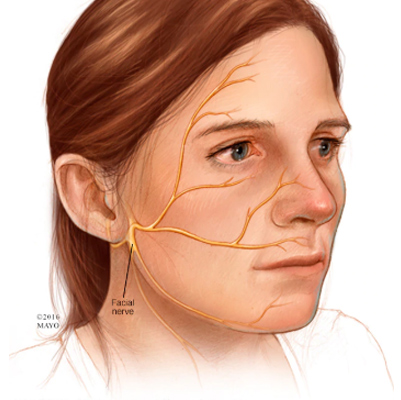
Ramsay Hunt Syndrome (Herpes Zoster Oticus)
Overview
Ramsay Hunt syndrome occurs when shingles (herpes zoster) affects the facial nerve (cranial nerve VII) near one of your ears.
It is caused by the varicella-zoster virus, the same virus that causes chickenpox. After chickenpox resolves, the virus can remain dormant in the nerves and reactivate years later. If it affects the facial nerve, it results in facial paralysis, ear pain, and sometimes hearing loss.
The rash and facial paralysis may appear simultaneously or one may precede the other, and occasionally the rash may not appear at all.
Symptoms
-
Painful red rash with fluid-filled blisters on, in, or around one ear
-
Facial weakness or paralysis on the affected side
-
Ear pain
-
Hearing loss
-
Tinnitus (ringing in the ears)
-
Difficulty closing one eye
-
Vertigo or dizziness
-
Changes in taste or loss of taste
-
Dry mouth and eyes
Effects
-
Permanent facial nerve damage if treatment is delayed
-
Partial or complete facial paralysis on the affected side
-
Persistent hearing loss or tinnitus
-
Balance problems due to inner ear involvement
-
Eye damage if the eye cannot close properly, leading to dryness or corneal injury
-
Emotional and social impact due to facial asymmetry or chronic pain
Treatment
1. Medications:
-
Antiviral drugs (e.g., acyclovir, valacyclovir) to reduce viral activity
-
Corticosteroids to reduce inflammation and nerve swelling
-
Pain relievers and sometimes neuropathic pain medications for nerve pain
2. Supportive Care:
-
Eye protection with lubricating drops or eye patches if eyelid closure is impaired
-
Physical therapy or facial exercises to maintain muscle tone and improve recovery
-
Balance therapy if vertigo is significant
3. Prognosis:
-
Early treatment (within 72 hours of symptom onset) improves recovery and reduces the risk of permanent nerve damage
-
Some patients may experience residual facial weakness, hearing loss, or chronic pain despite treatment
Tinnitus
Tinnitus
Overview
Tinnitus is the perception of noise or ringing in the ears without an external sound source. It affects approximately 15–20% of people.
Tinnitus is not a disease, but a symptom of an underlying condition, which may include:
-
Age-related hearing loss (presbycusis)
-
Ear injury or inner ear damage
-
Circulatory or cardiovascular disorders
-
Ear infections or wax buildup
Tinnitus can be temporary or chronic. While often annoying, it is not always a sign of a serious medical problem.
Symptoms
People with tinnitus may hear sounds such as:
-
Ringing
-
Buzzing
-
Roaring
-
Clicking
-
Hissing
-
Humming
Symptoms can be continuous or intermittent, affect one or both ears, and vary in intensity.
Effects / Complications
Chronic tinnitus can affect daily life, causing:
-
Difficulty concentrating
-
Sleep disturbances
-
Irritability or stress
-
Anxiety or depression
-
Reduced work or social functioning
Treatment / Management
Treatment aims to address the underlying cause and manage symptoms:
1. Medical Treatment
-
Treat underlying ear conditions (wax buildup, infections)
-
Manage cardiovascular or metabolic conditions contributing to tinnitus
2. Hearing Aids or Sound Therapy
-
Amplify external sounds to mask tinnitus
-
White noise machines or specialized sound generators
3. Medications
-
No specific drug for tinnitus, but some medications may reduce severity or related anxiety
4. Cognitive Behavioral Therapy (CBT)
-
Helps cope with emotional impact
-
Reduces stress and improves quality of life
5. Lifestyle and Home Remedies
-
Avoid loud noises
-
Reduce caffeine and alcohol intake
-
Manage stress
-
Use background noise to make tinnitus less noticeable

Tympanitis
Tympanitis
Overview
Tympanitis is the inflammation of the tympanic membrane (eardrum).
-
The tympanic membrane is a thin tissue that separates the outer ear from the middle ear and plays a crucial role in hearing by transmitting sound vibrations.
-
Inflammation can occur due to bacterial or viral infections, trauma, or fluid buildup in the middle ear.
-
Severe cases can affect hearing temporarily or, rarely, permanently if untreated.
Symptoms
Signs of tympanitis may include:
-
Ear pain in one or both ears
-
Fullness in the ear, often caused by fluid trapped behind a bulging eardrum
-
Bloody or watery discharge from the ear, especially if the eardrum ruptures
-
Hearing loss, usually temporary
-
Fever (possible, especially in infectious causes)
Effects / Complications
-
Temporary or permanent hearing impairment
-
Rupture of the eardrum in severe cases
-
Spread of infection to nearby structures, potentially causing middle ear or inner ear complications
Treatment / Management
-
Medical Management:
-
Antibiotics if bacterial infection is present
-
Analgesics for pain relief
-
Anti-inflammatory medications to reduce swelling
-
-
Supportive Care:
-
Keep the ear dry to prevent worsening infection
-
Avoid inserting objects into the ear
-
-
Surgical Intervention (if needed):
-
Myringotomy to drain fluid in severe cases
-
Tympanoplasty for eardrum repair if ruptured
-