Photophobia,
Phobias
Overview
Phobias are diagnosable mental disorders characterized by an exaggerated and irrational fear of a specific object, situation, or activity. Unlike normal fears, phobias are persistent, excessive, and disruptive, often causing intense anxiety even when there is little or no real danger.
Phobias can take various forms, such as:
-
Specific phobias: fear of animals, heights, flying, or injections
-
Social phobia (social anxiety disorder): fear of social situations or being judged
-
Agoraphobia: fear of being trapped in situations where escape may be difficult
People with phobias may go to great lengths to avoid the feared object or situation, which can significantly impact daily life and wellbeing.
Symptoms
Phobias trigger intense anxiety that can be physical, emotional, or cognitive, including:
-
Dizziness, trembling, or increased heart rate
-
Shortness of breath or hyperventilation
-
Nausea or stomach upset
-
A sense of unreality or detachment (derealization)
-
Fear of dying or catastrophic thoughts
-
Preoccupation with the feared object or situation
-
Avoidance behaviors that limit personal, social, or professional activities
Effects
-
Severe anxiety and panic attacks in the presence of the feared stimulus
-
Reduced quality of life due to avoidance of situations or activities
-
Difficulty maintaining relationships, work, or school responsibilities
-
Increased risk of depression, substance abuse, or other anxiety disorders
-
Physical health issues from chronic stress (e.g., high blood pressure, insomnia)
Treatment
Treatment is highly effective and aims to reduce fear, improve coping, and restore daily functioning:
1. Psychotherapy
-
Cognitive Behavioral Therapy (CBT): helps identify and change irrational thoughts and beliefs
-
Exposure therapy: gradual, controlled exposure to the feared object or situation to reduce anxiety
-
Acceptance and Commitment Therapy (ACT): helps manage fear without avoidance
2. Medications (used selectively)
-
Antidepressants (SSRIs, SNRIs) for long-term anxiety control
-
Benzodiazepines for short-term relief of acute anxiety (under medical supervision)
-
Beta-blockers for physical symptoms of anxiety in certain situations
3. Self-Help & Lifestyle Measures
-
Practice relaxation techniques (deep breathing, meditation, yoga)
-
Gradual exposure to feared situations in a safe environment
-
Support groups or counseling to share experiences and coping strategies

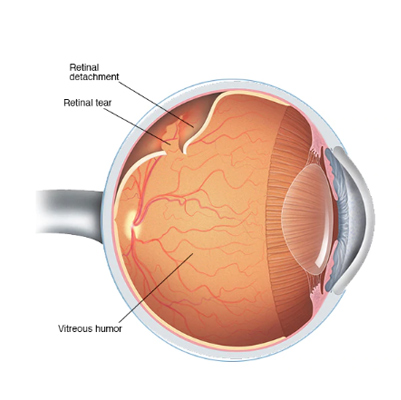
Retinal Detachment
Retinal Detachment
Overview
Retinal detachment is an ocular emergency in which a thin layer of tissue at the back of the eye—the retina—pulls away from its normal position.
The retina is essential for vision as it senses light and sends signals to the brain. When it detaches, the retinal cells are separated from the blood vessels that provide oxygen and nutrients, putting vision at serious risk.
If left untreated, retinal detachment can lead to permanent vision loss in the affected eye.
Symptoms
Although retinal detachment is typically painless, warning signs may appear before or during detachment:
-
Sudden increase in floaters (tiny specks drifting in your field of vision)
-
Flashes of light in one or both eyes (photopsia)
-
Blurred vision
-
Gradual loss of peripheral (side) vision
-
Appearance of a curtain or shadow over part of your visual field
Effects
-
Permanent vision loss if untreated
-
Impaired depth perception and central vision
-
Difficulty with daily activities, such as reading, driving, or recognizing faces
-
Psychological impact, including anxiety or depression due to vision impairment
Treatment
Retinal detachment requires urgent medical intervention. Treatment options include:
-
Laser therapy (photocoagulation)
-
Seals retinal tears before full detachment occurs
-
-
Cryopexy (freezing treatment)
-
Creates a scar to reattach the retina
-
-
Pneumatic retinopexy
-
Gas bubble injected into the eye to push the retina back into place
-
-
Scleral buckling
-
Silicone band placed around the eye to relieve retinal tension
-
-
Vitrectomy
-
Surgical removal of the vitreous gel to allow retina reattachment
-
Early detection and prompt treatment are critical to prevent permanent vision loss.
Swelling
Overview
A swollen eyelid occurs when there is inflammation or excess fluid (edema) in the connective tissues surrounding the eye. Swelling can affect both upper and lower eyelids and may be painful or painless.
-
It can result from allergies, infections, injuries, or systemic conditions.
-
A swollen eyelid may indicate a minor issue like seasonal allergies, or a serious eye infection requiring prompt treatment.
Symptoms
Swollen eyelids may present with:
-
Eye irritation (itchy, scratchy sensation)
-
Sensitivity to light (photophobia)
-
Excess tearing or watering of the eyes
-
Obstructed vision, depending on severity of swelling
-
Redness of the eyelid
-
Red eyes and conjunctival inflammation
-
Eye discharge or “mattering”
-
Eyelid dryness or flaking
-
Pain, especially if caused by infection
Effects / Complications
If untreated, a swollen eyelid can lead to:
-
Spread of infection (e.g., cellulitis or orbital infection)
-
Vision problems if swelling obstructs the eye
-
Corneal damage due to rubbing or exposure
-
Chronic discomfort or cosmetic issues
-
Rarely, systemic infection in severe cases
Treatment / Management
1. Home Care (for mild cases)
-
Apply a cold compress to reduce swelling
-
Avoid rubbing or touching the eye
-
Use over-the-counter antihistamines if due to allergies
-
Maintain eye hygiene, especially for discharge
2. Medical Treatment (for infection or severe swelling)
-
Topical or oral antibiotics for bacterial infections
-
Steroid eye drops for severe allergic reactions (under medical supervision)
-
Antiviral medication if caused by a viral infection
-
Drainage for styes or abscesses, if recommended by an ophthalmologist
3. Preventive Measures
-
Avoid exposure to allergens
-
Wash hands frequently and avoid touching eyes
-
Remove contact lenses when irritated
-
Treat underlying conditions like sinus infections or blepharitis

Dry Eyes Syndrome
Dry Eye Syndrome
Overview
One of the main functions of tears is to keep the eyes well-lubricated and protected. Dry Eye Syndrome occurs when your eyes do not produce enough tears or when the tears produced are of poor quality, leading to inadequate lubrication.
This condition can develop due to aging, autoimmune disorders (like Sjögren’s syndrome), thyroid imbalance, arthritis, lupus, or external factors such as pollution, smoke, prolonged screen time, air conditioning, or dry climates.
Dry eyes not only cause discomfort but may also lead to serious complications like corneal ulcers, scarring, or even vision loss if ignored.
Signs & Symptoms
People with dry eye syndrome may experience:
-
Burning, stinging, or scratchy sensation in the eyes
-
Eye redness
-
Sensitivity to light (photophobia)
-
Mucus production in or around the eyes
-
Blurred vision
-
Eye fatigue
-
Gritty feeling or “something stuck in the eye” sensation
-
Difficulty wearing contact lenses
-
Watery eyes (reflex tearing due to irritation)
-
Problems with nighttime driving
Effects
If untreated, dry eyes can lead to:
-
Constant eye discomfort and reduced quality of life
-
Recurrent eye infections
-
Inflammation of the cornea and conjunctiva
-
Corneal scarring or ulcers
-
Progressive vision problems
Treatment & Management
Lifestyle & Home Care
-
Limit screen time and follow the 20-20-20 rule (look 20 feet away for 20 seconds every 20 minutes)
-
Blink frequently, especially while reading or using gadgets
-
Stay hydrated and maintain a diet rich in omega-3 fatty acids
-
Use a humidifier in dry environments
-
Wear sunglasses or protective glasses outdoors
-
Wash eyes with clean water to remove dust and irritants
Medical Treatment
-
Artificial tears (eye drops) – to keep the eyes lubricated
-
Lubricating ointments or gels – for severe cases, especially at night
-
Anti-inflammatory eye drops – if caused by autoimmune disorders
-
Treating underlying systemic conditions such as thyroid disease, arthritis, or lupus
Homeopathic Treatment (By Spaks)
Homeopathy helps manage dryness, irritation, frequent infections, and burning sensations, aiming to improve tear quality and overall eye health.
? Common remedies (based on symptoms):
-
Euphrasia – for burning, watery eyes with sensitivity to light
-
Belladonna – for red, dry eyes with throbbing pain
-
Sulphur – for itchy, burning eyes worse in warm environments
-
Nux Vomica – for irritation caused by overuse of computers and stress
-
Pulsatilla – for thick mucus discharge and dryness, worse in warm rooms

Uveitis
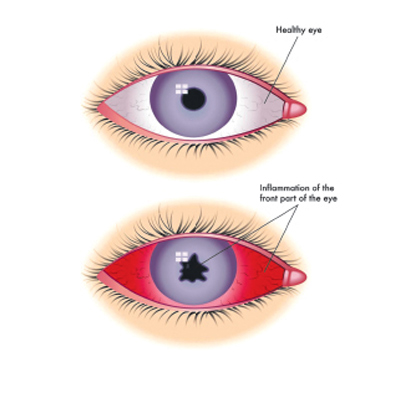
Uveitis
Overview
Uveitis is inflammation of the uvea, the middle layer of tissue in the eye wall. It can affect one or both eyes and may develop suddenly with symptoms worsening quickly.
-
Most commonly affects people aged 20–50, but children can also be affected.
-
Causes include infection, injury, autoimmune responses, or systemic diseases.
-
In many cases, the exact cause is unknown.
-
Early diagnosis and treatment are crucial to prevent complications, including permanent vision loss.
Symptoms
Signs and symptoms of uveitis may include:
-
Redness of the eye
-
Eye pain
-
Sensitivity to light (photophobia)
-
Blurred vision
-
Dark, floating spots in the field of vision (floaters)
-
Decreased vision
Effects / Complications
If left untreated, uveitis can lead to:
-
Permanent vision impairment or blindness
-
Glaucoma (increased eye pressure)
-
Cataracts
-
Retinal swelling or detachment
Treatment / Management
-
Medications:
-
Corticosteroid eye drops or oral steroids to reduce inflammation
-
Immunosuppressive drugs for autoimmune-related uveitis
-
Antibiotics or antivirals if infection is the cause
-
-
Eye Care:
-
Use of protective sunglasses to reduce light sensitivity
-
Regular eye check-ups to monitor pressure and retina health
-
-
Surgery:
-
Sometimes required for complications like cataracts or glaucoma
-
Vision Impairments
Vision Impairment
Overview
-
Vision impairment occurs when a person loses part or all of their ability to see, even when using corrective measures such as glasses, contact lenses, medication, or surgery.
-
It can be temporary or permanent, depending on the underlying cause.
-
The severity of vision impairment is classified into different types:
Types of Vision Impairments
-
Low Visual Acuity (Moderate Visual Impairment)
-
Visual acuity between 20/70 and 20/400 with best corrected vision
-
Visual field of no more than 20 degrees
-
-
Blindness
-
Complete or nearly complete loss of vision
-
-
Legal Blindness (varies by country)
-
In the United States, defined as:
-
Visual acuity of 20/200 or worse with best corrected vision
-
Visual field of no more than 20 degrees
-
-
Symptoms
-
Severe or sudden eye pain
-
Recurrent pain in or around the eye
-
Blurred or double vision
-
Seeing flashes of light or sudden bright floating spots
-
Seeing rainbows or halos around lights
-
Seeing floating “spider webs”
-
Seeing a “curtain coming down” over one eye
-
Unusual or painful sensitivity to light (photophobia)
-
Swollen or red eyes
-
Changes in iris color
-
White areas in the pupil of the eye
Effects / Complications
-
Difficulty performing daily activities (reading, driving, recognizing faces)
-
Loss of independence
-
Increased risk of accidents or falls
-
Psychological impact, including depression and anxiety
Treatment / Management
-
Corrective lenses (glasses or contact lenses)
-
Medication or surgery for treatable conditions (e.g., cataracts, glaucoma)
-
Assistive devices (magnifiers, screen readers, braille materials)
-
Vision rehabilitation to maximize remaining vision
-
Lifestyle adaptations to maintain safety and independence
