Intercostal neuralgia
Intercostal Neuralgia
Overview
Intercostal neuralgia is a type of nerve pain that affects the intercostal nerves — the nerves running between your ribs, branching from the spinal cord. This condition usually causes thoracic (chest wall) pain, which may spread across the upper trunk.
Sometimes, pain in this region may also come from intercostal muscle strain, which occurs when the muscles between two or more ribs are overstretched, twisted, or torn. These muscles are important for building the chest wall and assisting in breathing, so injury or irritation can cause significant discomfort.
Symptoms
The primary symptom of intercostal neuralgia is burning, sharp, or shooting pain. This pain may be felt:
-
Around the ribs
-
In the upper chest
-
In the upper back
Additional symptoms include:
-
Squeezing or pressure-like pain wrapping around the chest from front to back
-
Tingling sensation
-
Numbness in affected areas
Effects
-
Difficulty in breathing deeply due to pain
-
Pain worsening with movement, coughing, or sneezing
-
Reduced physical activity due to discomfort
-
Sleep disturbances from persistent pain
-
Anxiety or stress caused by chronic pain
Homeopathic Treatment
-
Arnica montana – for intercostal pain after injury, strain, or trauma
-
Bryonia alba – for sharp stitching pain in the chest, worse on movement or deep breathing
-
Ranunculus bulbosus – for burning or shooting intercostal pain with muscle sensitivity
-
Hypericum perforatum – for nerve pain with tingling and numbness
-
Magnesia phosphorica – for cramping or radiating chest wall pain, relieved by warmth

Joint Pain
Joint Pain
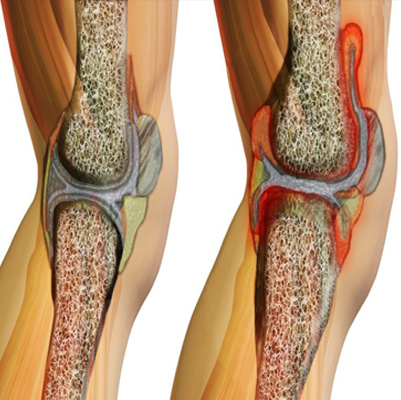
Overview
Joints are the parts of your body where bones connect, allowing movement and flexibility. Major joints include the shoulders, hips, elbows, and knees.
Joint pain refers to discomfort, aches, or soreness in one or more of these joints. It is a common complaint and often does not require hospital treatment. However, in some cases, it may be a sign of an underlying condition or injury.
One of the most common causes of joint pain is arthritis, but other health problems, injuries, infections, or overuse can also lead to joint discomfort.
Symptoms
-
Redness around the joint
-
Swelling
-
Tenderness or pain when touched
-
Warmth in the joint area
-
Limping or difficulty walking
-
Joint stiffness
-
Weakness in the joint
-
Locking of the joint
-
Loss of range of motion
Effects
If untreated or chronic, joint pain can lead to:
-
Reduced ability to move or perform daily tasks
-
Muscle weakness and stiffness
-
Sleep disturbances due to pain
-
Long-term joint damage or deformity (especially with arthritis)
-
Emotional effects such as stress, anxiety, or depression
Treatment
Self-care & Lifestyle:
-
Rest and avoid activities that strain the affected joint
-
Apply hot or cold compresses to reduce pain and swelling
-
Maintain a healthy weight to reduce pressure on joints
-
Gentle stretching and low-impact exercises (like swimming, yoga, or walking)
-
Use supportive devices (braces, canes, or orthotics) if needed
Medical Treatments:
-
Over-the-counter pain relievers (acetaminophen, ibuprofen, naproxen)
-
Anti-inflammatory medications (NSAIDs)
-
Topical creams or gels for localized relief
-
Corticosteroid injections for severe inflammation
-
Physical therapy to improve strength and flexibility
-
Surgery (joint replacement or repair) in severe cases

Juvenile idiopathic arthritis
Juvenile Arthritis (Juvenile Idiopathic Arthritis)
Overview
Juvenile arthritis, earlier called juvenile rheumatoid arthritis, is the most common type of arthritis in children under the age of 16.
It causes persistent joint pain, swelling, and stiffness. For some children, symptoms may last only a few months, while for others, the condition may continue into adulthood.
Certain types of juvenile arthritis can lead to serious complications, such as growth problems, joint damage, and eye inflammation. Early treatment is crucial to control pain, reduce inflammation, improve function, and prevent long-term disability.
Symptoms
-
Pain – Children may not complain directly, but you may notice limping, especially in the morning or after naps.
-
Swelling – Often seen first in larger joints, like the knee.
-
Stiffness – The child may appear clumsy or have difficulty moving after rest.
-
Fever, swollen lymph nodes, and rash – In some cases, a high fever, swollen glands, or a rash on the trunk, usually worse in the evenings.
Effects
If left untreated, juvenile arthritis can cause:
-
Permanent joint damage or deformity
-
Slow or uneven bone growth in children
-
Eye inflammation (uveitis), which may lead to vision problems
-
Fatigue and difficulty with daily activities
-
Emotional and social challenges due to chronic illness
Treatment
Medical Treatment:
-
Nonsteroidal anti-inflammatory drugs (NSAIDs) – to reduce pain and inflammation
-
Disease-modifying antirheumatic drugs (DMARDs) – such as methotrexate, to control disease progression
-
Biologic agents – for children who don’t respond to other medicines
-
Corticosteroids – for severe inflammation, though used with caution due to side effects
Lifestyle & Supportive Care:
-
Physical therapy & exercise – to maintain mobility and strength
-
Healthy diet – to support growth and reduce inflammation
-
Regular eye checkups – to detect and treat eye inflammation early
-
Emotional support – counseling and support groups for children and families
Knee Pain
Knee Pain
Overview
Knee pain is a common problem that can affect people of all ages. It may result from an injury, such as a torn cartilage or damaged ligament, or from medical conditions like arthritis, gout, and infections.
The knee is the joint between the bones of the upper and lower leg. It allows the leg to bend, provides stability to support body weight, and helps in essential movements such as walking, running, crouching, jumping, and turning.
Symptoms
Signs and symptoms of knee pain may include:
-
Swelling and stiffness
-
Redness and warmth to the touch
-
Weakness or instability
-
Popping or crunching noises
-
Inability to fully straighten the knee
Effects
If untreated, knee pain can lead to:
-
Difficulty walking or climbing stairs
-
Reduced mobility and flexibility
-
Chronic joint damage or deformity
-
Muscle weakness around the knee
-
Long-term disability in severe cases
Treatment
Treatment depends on the cause and severity of pain, and may include:
-
Rest and Ice: To reduce swelling and pain after injury
-
Medications: Pain relievers and anti-inflammatory drugs
-
Physical Therapy: Strengthening muscles around the knee to improve stability
-
Supportive Devices: Knee braces or orthotics for extra support
-
Injections: Corticosteroid or hyaluronic acid injections in severe cases
-
Surgery: Procedures like arthroscopy, ligament repair, or knee replacement (in advanced conditions)

Leg Pain
Leg Pain
Overview
Leg pain can occur due to issues in any part of the leg — including skin, bones, muscles, tendons, nerves, or blood vessels. The causes range from injuries (fractures, sprains, strains) to infections, arthritis, vascular disease, or blood clots.
Leg pain may affect one leg or both, depending on the underlying cause, and its intensity can range from mild to severe.
Symptoms
-
Pain that may feel sharp, dull, numbing, tingling, burning, radiating, or aching
-
Pain triggered by nerve response to pressure, temperature changes, or chemical release from tissue damage
-
Swelling, redness, or warmth (if infection or inflammation is present)
-
Stiffness or weakness in the leg
-
Difficulty walking or bearing weight
Effects
If untreated, leg pain can lead to:
-
Reduced mobility and difficulty in daily activities
-
Persistent swelling and discomfort
-
Risk of complications like blood clots, chronic arthritis, or nerve damage
-
Sleep disturbances due to pain at night
Treatment
Management depends on the underlying cause:
-
Rest and elevation of the leg to reduce swelling and strain
-
Cold or warm compresses for pain relief
-
Pain relievers or anti-inflammatory medicines (NSAIDs)
-
Compression stockings for venous or blood circulation issues
-
Physiotherapy to strengthen muscles and improve mobility
-
Antibiotics if the cause is infection
-
Surgery may be required for fractures, severe vascular disease, or blood clots
Self-care tips:
-
Maintain a healthy weight to reduce strain on the legs
-
Exercise regularly to improve blood flow and muscle strength
-
Avoid standing or sitting for long periods without movement

Neck and shoulders Pain
Neck and Shoulder Pain
Overview
The neck and shoulders contain a complex network of muscles, bones, nerves, arteries, veins, ligaments, and other supporting structures. Because of this, many different conditions can lead to pain in this area.
Neck pain is a very common complaint. It often results from muscle strain due to poor posture, such as leaning over a laptop, looking down at a phone, or hunching at a work desk. Other causes include osteoporosis, arthritis, injuries, or degenerative changes.
While most neck pain is not serious, in rare cases it may indicate a more severe underlying condition. Medical attention should be sought if neck pain is accompanied by numbness, weakness in arms or hands, or shooting pain that radiates into the shoulders or arms.
Symptoms
Common signs and symptoms include:
-
Persistent pain, often worsened by keeping the head in one position (e.g., driving or computer work)
-
Muscle tightness, stiffness, or spasms
-
Reduced range of motion in the neck
-
Headaches (often starting at the base of the skull and radiating forward)
-
Shoulder pain or discomfort that may radiate into the arms

Osteoarthritis
Overview
Osteoarthritis is the most common form of arthritis, affecting millions of people worldwide. It occurs when the protective cartilage that cushions the ends of bones gradually wears down over time. Without this cartilage, bones begin to rub against each other, causing pain, swelling, and reduced movement.
Although osteoarthritis can damage any joint in the body, it most commonly affects the hands, knees, hips, and spine.
While the disease process itself cannot be reversed, symptoms can usually be managed effectively. Lifestyle changes, maintaining a healthy weight, exercise, and medical treatments may help slow progression, relieve pain, and improve joint function. Symptoms usually develop gradually and worsen over time.
Symptoms of Osteoarthritis
-
Pain: Joint pain during or after movement
-
Tenderness: Sensitivity when light pressure is applied to the joint
-
Stiffness: Most noticeable in the morning or after long periods of inactivity
-
Loss of flexibility: Reduced ability to move the joint fully
-
Grating sensation: A grinding or crackling sound/feeling during movement
-
Bone spurs: Hard lumps of extra bone that may form around the joint
-
Swelling: Inflammation in or around the affected joint
Effects
-
Chronic pain that may limit physical activity and mobility
-
Reduced independence, as daily tasks (walking, climbing stairs, gripping objects) become difficult
-
Increased risk of disability and joint deformity in advanced cases
-
Emotional and psychological impact, such as depression, stress, or anxiety due to chronic pain
-
Greater risk of falls or injuries due to joint instability and stiffness
Treatment
Although there is no cure for osteoarthritis, a combination of lifestyle changes and medical treatments can help manage symptoms:
1. Lifestyle Modifications
-
Regular exercise (low-impact activities like walking, swimming, yoga) to strengthen muscles and improve flexibility
-
Weight management to reduce stress on weight-bearing joints (knees, hips, spine)
-
Use of assistive devices (canes, braces, supportive footwear) to reduce joint strain
2. Medications
-
Over-the-counter pain relievers (acetaminophen, NSAIDs like ibuprofen)
-
Prescription stronger painkillers or anti-inflammatories in severe cases
-
Topical creams/gels with analgesics or anti-inflammatory agents
3. Therapies
-
Physical therapy to improve joint function and strengthen surrounding muscles
-
Occupational therapy to adapt daily tasks and protect joints
4. Medical Procedures
-
Injections: Corticosteroids or hyaluronic acid injections to relieve pain and improve mobility
-
Surgery (for advanced cases):
-
Joint replacement (hip or knee arthroplasty)
-
Realignment of bones (osteotomy)
-
Joint fusion (arthrodesis) for smaller joints
-
5. Prevention & Self-care
-
Avoid repetitive joint strain
-
Maintain proper posture
-
Include joint-friendly foods (rich in omega-3, calcium, vitamin D)

Osteoporosis
Overview
Osteoporosis is a bone disease that causes bones to become weak, brittle, and fragile. In this condition, even minor stresses — such as bending, coughing, or a simple fall — can cause fractures. The most common fracture sites are the hip, spine, and wrist.
Bones are living tissue that constantly break down (resorption) and rebuild (formation). Osteoporosis develops when the body cannot make enough new bone to keep up with the breakdown of old bone.
While osteoporosis can affect both men and women of all races, postmenopausal women, particularly those who are white or Asian, are at the highest risk. Preventive measures like proper medications, a healthy diet, and regular weight-bearing exercise can help slow or even reverse bone loss.
Symptoms of Osteoporosis
Osteoporosis is often called the “silent disease” because it develops slowly and shows no symptoms in its early stages. Once bones have weakened, signs may include:
-
Back pain due to a collapsed or fractured vertebra
-
Loss of height over time
-
Stooped posture (kyphosis or hunchback)
-
Bone fractures that occur more easily than expected (even from minor falls or stresses)
Effects
-
Increased risk of fractures, particularly in the hip and spine, which can lead to long-term disability
-
Chronic pain and immobility following fractures
-
Decreased independence, as mobility and daily activities may become limited
-
Emotional and psychological impact, such as fear of falling, anxiety, or depression
-
In severe cases, hip or spinal fractures can significantly increase the risk of premature mortality in older adults
Treatment
While osteoporosis cannot be completely cured, it can be managed to reduce fracture risk and strengthen bones:
1. Lifestyle & Self-care
-
Diet rich in calcium and vitamin D (milk, leafy greens, fortified foods, sunlight exposure)
-
Regular weight-bearing and muscle-strengthening exercises (walking, jogging, dancing, resistance training)
-
Quit smoking and limit alcohol intake, as both accelerate bone loss
2. Medications
-
Bisphosphonates (alendronate, risedronate) – slow bone loss
-
Selective Estrogen Receptor Modulators (SERMs) – protect bone in postmenopausal women
-
Hormone-related therapy (estrogen or testosterone, in select cases)
-
Denosumab or teriparatide – newer options for severe cases
3. Preventing Falls
-
Use of assistive devices like canes or walkers if balance is poor
-
Fall-proofing the home (removing rugs, installing handrails, ensuring good lighting)
4. Surgery (for fractures)
-
Vertebroplasty or kyphoplasty for spinal fractures
-
Hip replacement surgery if necessary
