Plantar fasciitis (Pain in sole)
Plantar Fasciitis
Overview
Plantar fasciitis is one of the most common causes of heel pain. It involves inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of the foot, connecting the heel bone to the toes.
The condition typically causes stabbing pain, especially with the first steps in the morning. The pain often decreases as you move around, but may return after long periods of standing or after sitting.
Plantar fasciitis is more common in runners and in individuals who are overweight or wear shoes with poor support.
Symptoms
-
Stabbing pain at the bottom of the foot near the heel
-
Pain worst during the first few steps in the morning
-
Pain triggered by long periods of standing or rising from sitting
-
Heel pain that may worsen with exercise (especially at the start, not during activity)
-
Foot stiffness and tenderness
Effects
-
Chronic pain affecting walking, standing, and daily activities
-
Difficulty performing exercises or sports, limiting mobility
-
Altered gait or posture to compensate for pain, which may lead to additional musculoskeletal issues
-
Emotional and quality-of-life impact due to persistent discomfort
Treatment
1. Conservative Measures:
-
Rest and activity modification to reduce stress on the heel
-
Ice therapy to reduce inflammation and pain
-
Stretching exercises for the plantar fascia, Achilles tendon, and calf muscles
-
Supportive footwear with cushioned soles and arch support
-
Orthotic inserts to distribute pressure evenly across the foot
2. Medications:
-
Over-the-counter pain relievers and anti-inflammatory medications (e.g., ibuprofen)
3. Physical Therapy:
-
Targeted exercises to strengthen foot and lower leg muscles
-
Techniques like massage, ultrasound, or taping for pain relief
4. Advanced Treatments (if conservative care fails):
-
Corticosteroid injections to reduce severe inflammation
-
Extracorporeal shock wave therapy in chronic cases
-
Surgical intervention (rare) to release tension in the plantar fascia

Polymyalgia rheumatica
Polymyalgia Rheumatica (PMR)
Overview
Polymyalgia rheumatica (PMR) is an inflammatory disorder that primarily causes muscle pain and stiffness, especially in the shoulders, neck, hips, and thighs.
Symptoms usually develop rapidly and are worse in the morning or after periods of inactivity. PMR mainly affects people over 65 years old and is rare in those under 50.
PMR is associated with giant cell arteritis, another inflammatory condition affecting blood vessels, which can cause headaches, vision problems, jaw pain, and scalp tenderness. Some people may have both conditions simultaneously.
Symptoms
PMR symptoms typically occur on both sides of the body and include:
-
Pain in the shoulders
-
Aches or stiffness in the neck, upper arms, hips, or thighs
-
Stiffness, especially in the morning or after inactivity
-
Limited range of motion in affected areas
-
Pain and stiffness in the wrists, elbows, or knees
-
Fatigue or general malaise in some cases
Effects
-
Reduced mobility and difficulty performing daily activities
-
Persistent pain and stiffness, affecting quality of life
-
Increased risk of giant cell arteritis, which can cause vision loss if untreated
-
Emotional and psychological impact due to chronic discomfort
-
Potential muscle weakness if symptoms persist without treatment
Treatment
1. Medications:
-
Corticosteroids (e.g., prednisone) are the main treatment to reduce inflammation and relieve symptoms
-
Nonsteroidal anti-inflammatory drugs (NSAIDs) for mild symptom relief
-
Immunosuppressive medications in rare or resistant cases
2. Lifestyle Measures:
-
Gentle exercise and stretching to maintain mobility
-
Physical therapy to improve strength and range of motion
-
Balanced diet to support overall health and reduce inflammation
3. Monitoring and Follow-Up:
-
Regular check-ups to monitor inflammatory markers and adjust medications
-
Screening for giant cell arteritis to prevent complications such as vision loss

psoriatic arthritis
Psoriatic Arthritis (PsA)
Overview
Psoriatic arthritis (PsA) is a chronic inflammatory arthritis that affects the joints and surrounding tissues. It typically occurs in people who already have psoriasis, a skin condition causing red, scaly patches on areas such as the elbows, knees, back, buttocks, and scalp.
In some cases, joint symptoms may appear before the skin symptoms, and some individuals with PsA never develop psoriasis. PsA can affect any adult, regardless of gender, and occasionally children.
Symptoms
Common symptoms of psoriatic arthritis include:
-
Pain, swelling, and stiffness in and around the joints
-
Swollen fingers or toes (dactylitis) due to inflammation in joints and tendons
-
Stiff back or neck (spondylitis) from spinal inflammation
-
Heel pain from inflammation where the Achilles tendon attaches to bone
-
Pain in other tendon attachment sites (enthesitis), such as knees, hips, or chest
-
Nail changes, including pitting, thickening, or discoloration
-
Fatigue, caused by inflammation and the emotional impact of living with a chronic disease
Effects
-
Joint damage and deformity if inflammation is untreated
-
Reduced mobility and difficulties performing daily activities
-
Chronic pain and stiffness, affecting quality of life
-
Emotional distress, including anxiety or depression from living with a long-term illness
-
Increased risk of cardiovascular disease due to chronic systemic inflammation
Treatment
1. Medications:
-
Nonsteroidal anti-inflammatory drugs (NSAIDs) to relieve pain and inflammation
-
Disease-modifying antirheumatic drugs (DMARDs), such as methotrexate, to slow disease progression
-
Biologic therapies (e.g., TNF inhibitors) for moderate to severe cases
-
Corticosteroids for short-term control of inflammation
2. Lifestyle Measures:
-
Regular exercise and physical therapy to maintain joint flexibility and strength
-
Healthy diet to reduce inflammation and support overall health
-
Stress management to help cope with chronic pain
3. Supportive Care:
-
Occupational therapy to improve function in daily activities
-
Pain management techniques for chronic discomfort

Raynaud's Phenomenon
Raynaud's Phenomenon
Overview
Raynaud's Phenomenon is a condition in which certain areas of the body—commonly the fingers and toes—become numb, cold, and discolored in response to cold temperatures or emotional stress.
In this condition, the small arteries that supply blood to the skin constrict (vasospasm), limiting blood flow to the affected areas.
Women are more likely than men to develop Raynaud's Phenomenon, and it is more common in people living in colder climates. The condition can occur on its own (primary Raynaud's) or as part of another disease (secondary Raynaud's), such as autoimmune disorders.
While the condition is rarely disabling, it can affect quality of life and, in severe cases, may lead to skin damage.
Symptoms
-
Cold fingers or toes
-
Color changes in the skin in response to cold or stress (white → blue → red)
-
Tingling, prickly sensation, or stinging pain upon warming or stress relief
-
In severe cases: ulcers or sores on the fingertips or toes
Effects
-
Discomfort and pain during attacks
-
Reduced dexterity in fingers due to numbness
-
Skin ulcers or infections in severe cases of secondary Raynaud's
-
Long-term tissue damage if blood flow is severely restricted
-
Impact on daily activities and quality of life
Treatment
1. Lifestyle and Self-Care:
-
Keep hands and feet warm, wear gloves and socks
-
Avoid smoking and limit caffeine, as these can worsen vasospasms
-
Stress management techniques to reduce frequency of attacks
2. Medications:
-
Vasodilators (e.g., calcium channel blockers) to improve blood flow
-
Topical nitrates to relax small blood vessels in severe cases
-
Medications for underlying conditions if Raynaud's is secondary
3. Advanced Therapies (for severe cases):
-
Surgical interventions such as sympathectomy to improve blood flow
-
Treatment of skin ulcers or infections if present
4. Monitoring:
-
Regular checkups for secondary Raynaud's to prevent complications
-
Early treatment of any skin sores or tissue damage

Repetative Stress Injury
Repetitive Stress Injury (RSI)
Overview
Repetitive Stress Injury (RSI) refers to a group of conditions that occur when muscles, tendons, and nerves are overused or strained due to repetitive motions, sustained awkward positions, forceful exertions, or mechanical compression.
RSIs can affect any movable part of the body, but they are most common in the hands, wrists, elbows, shoulders, and neck. Common causes include:
-
Extended use of computers or laptops
-
Typing or texting for long periods
-
Assembly line work or manual labor
-
Sports involving repetitive motion
Other names for RSI include:
-
Repetitive motion disorder (RMD)
-
Cumulative trauma disorder (CTD)
-
Occupational overuse syndrome
-
Regional musculoskeletal disorder
Symptoms
Symptoms of RSI can vary depending on the affected area, but common signs include:
-
Tenderness or pain in the affected muscle or joint
-
Throbbing or pulsating sensation in the area
-
Tingling or numbness, often in the hands or arms
-
Loss of sensation or reduced grip strength
-
Swelling, stiffness, or limited range of motion
Effects
-
Chronic pain and discomfort in affected areas
-
Reduced strength and mobility, making daily tasks difficult
-
Nerve damage in severe cases (e.g., carpal tunnel syndrome)
-
Decreased productivity at work or during activities
-
Long-term joint or tendon degeneration if untreated
Treatment
1. Rest and Activity Modification:
-
Take frequent breaks from repetitive tasks
-
Avoid movements that exacerbate pain
2. Physical Therapy and Exercises:
-
Stretching and strengthening exercises for muscles and tendons
-
Ergonomic adjustments for workstations (keyboard, mouse, chair)
3. Pain Relief:
-
NSAIDs or over-the-counter pain relievers for inflammation
-
Ice or heat therapy to reduce pain and swelling
4. Supportive Devices:
-
Wrist splints or braces to reduce strain
-
Ergonomic keyboards, mouse pads, and chairs
5. Advanced Treatments:
-
Corticosteroid injections for severe inflammation
-
Surgery in rare cases to relieve nerve compression

Restless legs syndrome
Restless Legs Syndrome (RLS/WED)
Overview
Restless Legs Syndrome (RLS), also known as Willis-Ekbom Disease (WED), is a neurological disorder that causes an uncontrollable urge to move the legs, often accompanied by uncomfortable sensations.
These sensations typically occur:
-
During periods of rest (sitting or lying down)
-
In the evening or nighttime hours
Movement temporarily relieves the discomfort, which can significantly disrupt sleep and interfere with daily life. RLS can begin at any age and often worsens as a person gets older.
RLS is sometimes associated with Periodic Limb Movement of Sleep (PLMS), a condition in which the legs twitch involuntarily during sleep.
Symptoms
The primary symptom is the urge to move the legs, often accompanied by:
-
Unpleasant sensations in the legs (tingling, crawling, itching, burning, or aching)
-
Symptoms that begin or worsen during rest
-
Temporary relief with movement (stretching, pacing, or walking)
-
Symptoms that worsen in the evening or at night
-
Nighttime leg twitching or involuntary jerks
-
Difficulty falling asleep or staying asleep due to discomfort
Effects
-
Sleep disruption leading to fatigue, daytime sleepiness, and reduced concentration
-
Impaired work performance and daily functioning
-
Emotional stress, anxiety, or depression due to chronic sleep loss
-
Worsening of coexisting medical conditions such as cardiovascular disease
Treatment
1. Lifestyle and Self-Care:
-
Maintain regular sleep patterns
-
Exercise moderately during the day (avoid vigorous exercise in the evening)
-
Reduce caffeine, alcohol, and nicotine
-
Warm baths, leg massages, or heating pads to relieve discomfort
-
Use of compression stockings or pneumatic compression devices in some cases
2. Medications:
-
Dopaminergic agents (e.g., pramipexole, ropinirole) to reduce leg sensations
-
Anti-seizure medications (e.g., gabapentin, pregabalin) for nerve-related discomfort
-
Opioids or benzodiazepines in severe cases
-
Iron supplements if RLS is associated with iron deficiency
3. Management of Underlying Conditions:
-
Treating kidney disease, diabetes, or neuropathy if present
-
Correcting vitamin or mineral deficiencies
With proper treatment and lifestyle adjustments, most people with RLS can manage symptoms and improve sleep quality.

Rheumatoid arthritis
Rheumatoid Arthritis (RA)
Overview
Rheumatoid arthritis is a chronic inflammatory autoimmune disorder that primarily affects the joints, but it can also impact other organ systems, including the skin, eyes, lungs, heart, and blood vessels.
In RA, the immune system mistakenly attacks the body’s tissues, especially the synovium (the lining of the joints). This leads to painful swelling, inflammation, and stiffness, which can eventually cause bone erosion and joint deformity. Unlike osteoarthritis, which is caused by wear-and-tear, RA is an autoimmune disease.
Symptoms
-
Tender, warm, swollen joints
-
Joint stiffness, usually worse in the morning or after periods of inactivity
-
Fatigue
-
Fever
-
Loss of appetite
-
Persistent low-grade fever
Effects / Complications
If left untreated, RA can lead to:
-
Joint deformities and loss of function
-
Osteoporosis (weakening of bones)
-
Rheumatoid nodules (firm lumps under the skin)
-
Cardiovascular problems (increased risk of heart attack and stroke)
-
Lung disease (inflammation or scarring)
-
Eye complications (dry eyes, scleritis, or uveitis)
-
Anemia or other blood disorders
Treatment
RA treatment aims to control inflammation, relieve symptoms, prevent joint and organ damage, and maintain quality of life:
-
Medications
-
NSAIDs (e.g., ibuprofen) for pain and inflammation
-
Corticosteroids to reduce inflammation quickly
-
Disease-modifying antirheumatic drugs (DMARDs) such as methotrexate to slow disease progression
-
Biologic agents (e.g., TNF inhibitors) for moderate to severe RA
-
-
Physical Therapy
-
Exercises to maintain joint flexibility and strengthen muscles
-
-
Lifestyle Changes
-
Regular low-impact exercise
-
Balanced diet rich in anti-inflammatory foods
-
Joint protection strategies
-
-
Surgery (in severe cases)
-
Joint repair, replacement, or fusion
-
Early diagnosis and treatment are crucial to prevent irreversible joint damage and disability.

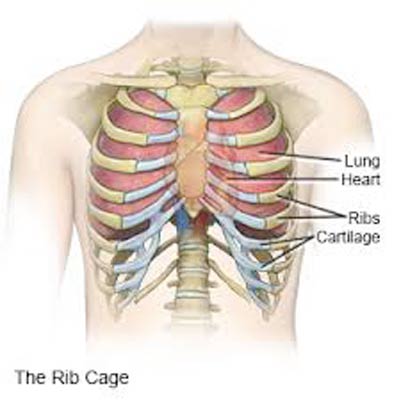
Pain in Ribs
Rib Cage Pain
Overview
Rib cage pain can feel sharp, dull, achy, or stabbing and is typically felt at or below the chest or above the navel on either side. It may occur after a clear injury (such as trauma or accident) or sometimes without an obvious cause.
This pain may arise from:
-
Muscle strain (from heavy lifting, exercise, or coughing)
-
Joint inflammation (such as costochondritis, inflammation of cartilage connecting ribs to the breastbone)
-
Rib fracture or bruising from injury
-
Chronic pain conditions affecting the chest wall
Rib cage pain can sometimes mimic or overlap with pain from lung, heart, or gastrointestinal issues, so proper evaluation is important.
Symptoms
-
Shortness of breath
-
Rapid breathing
-
Coughing (sometimes with blood)
-
Anxiety or restlessness
-
Lightheadedness or dizziness
-
Sweating
-
Irregular heartbeat
-
Localized tenderness, swelling, or bruising in some cases
Effects
-
Mild cases (muscle strain or bruising) often improve with rest but may limit daily activity temporarily.
-
Severe cases (rib fracture or lung involvement) can lead to:
-
Difficulty breathing and reduced lung capacity
-
Risk of collapsed lung (pneumothorax) or infection (pneumonia)
-
Chronic pain if not treated properly
-
-
May cause significant anxiety because chest pain is often linked to heart or lung disease.
Treatment
Treatment depends on the underlying cause:
1. Home & Supportive Care
-
Rest and avoid activities that worsen pain
-
Apply ice packs to reduce swelling/bruising in case of injury
-
Over-the-counter pain relievers (acetaminophen, ibuprofen)
-
Gentle breathing exercises to maintain lung capacity
2. Medical Treatment
-
For costochondritis: anti-inflammatory medicines, physical therapy
-
For rib fractures: pain control, supportive bandaging, sometimes hospitalization
-
For lung-related causes (like pneumothorax or pulmonary embolism): urgent medical intervention, oxygen therapy, or surgery
-
If infection (pneumonia) is suspected: antibiotics and supportive care
3. Lifestyle & Prevention
-
Practice safe lifting techniques
-
Use protective gear during contact sports
-
Avoid smoking (reduces risk of lung complications)
-
Maintain strong core and chest muscles through regular exercise