Sciatica
Sciatica
Overview
Sciatica refers to pain that radiates along the path of the sciatic nerve, which branches from the lower back through the hips, buttocks, and down each leg.
-
Usually affects one side of the body.
-
Most commonly caused by compression of the nerve due to:
-
Herniated disc
-
Bone spur on the spine
-
Spinal stenosis (narrowing of the spine)
-
-
Compression leads to inflammation, pain, and other neurological symptoms in the affected leg.
Symptoms
-
Lower back pain
-
Pain in the buttocks or leg, often worse when sitting
-
Hip pain
-
Burning or tingling sensation down the leg
-
Weakness, numbness, or difficulty moving the leg
-
Persistent pain on one side of the lower back
-
Foot pain that makes it difficult to stand or walk
Effects / Complications
-
Chronic pain if untreated
-
Reduced mobility and difficulty performing daily activities
-
Muscle weakness in the leg or foot
-
Nerve damage in severe or prolonged cases
-
Impact on quality of life, including sleep disturbances and emotional stress
Treatment
1. Self-Care / Lifestyle Measures
-
Rest (short-term) and avoiding prolonged sitting
-
Gentle stretches and physical therapy exercises to strengthen the back and core
-
Hot or cold compresses to reduce pain and inflammation
2. Medications
-
Pain relievers: acetaminophen
-
Nonsteroidal anti-inflammatory drugs (NSAIDs): ibuprofen, naproxen
-
Muscle relaxants if muscle spasms are present
-
Prescription medications for severe nerve pain
3. Interventional Treatments
-
Corticosteroid injections near the affected nerve to reduce inflammation
-
Nerve blocks in select cases
4. Surgery (in severe or persistent cases)
-
Microdiscectomy or laminectomy to relieve nerve compression
-
Recommended when pain is severe, persistent, or associated with progressive weakness or loss of bowel/bladder control

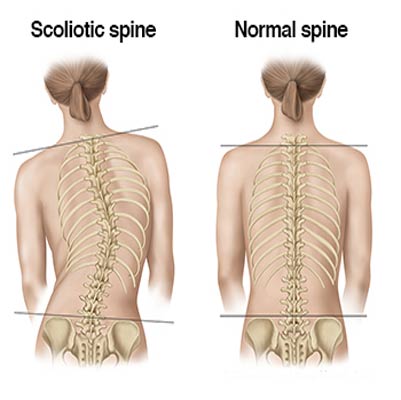
Scoliosis Disease
Scoliosis
Overview
Scoliosis is a sideways curvature of the spine, most commonly developing during the growth spurt just before puberty.
-
The cause is unknown in most cases (idiopathic scoliosis).
-
Some cases are linked to neurological disorders, genetic conditions, or congenital spinal deformities.
-
Mild scoliosis may not cause significant problems, but severe curvature can:
-
Lead to disabling deformities
-
Reduce the space within the chest, making breathing difficult
-
Symptoms
-
One shoulder higher than the other
-
Prominent shoulder blade on one side
-
Uneven hips
-
Rotating spine (rib hump visible when bending forward)
-
Hip pain
-
Breathing difficulties in severe cases due to reduced chest space
Effects / Complications
-
Back pain
-
Physical deformity and asymmetry
-
Reduced lung function in severe curves
-
Chronic discomfort or disability in untreated severe scoliosis
-
Emotional and social impact due to visible spinal deformity
Treatment
1. Observation / Monitoring
-
Mild scoliosis is often monitored regularly through X-rays.
-
Growth and curvature progression are checked periodically.
2. Bracing
-
Used for moderate scoliosis to prevent further curvature
-
Most effective in children and adolescents who are still growing
3. Physical Therapy
-
Strengthens spinal muscles
-
Improves posture and flexibility
-
May reduce back pain
4. Surgery
-
Recommended for severe scoliosis or progressive curves
-
Spinal fusion is the most common surgical procedure
-
Surgery corrects curvature, stabilizes the spine, and prevents further progression
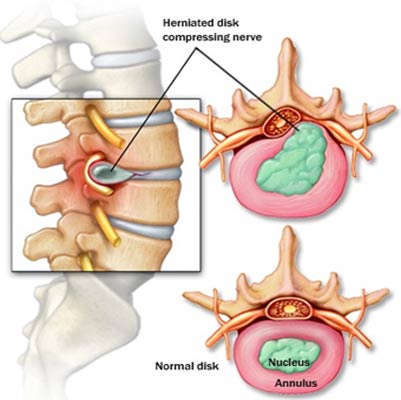
Slipped disk
Slipped Disk (Herniated Disk)
Overview
A slipped disk refers to a problem with one of the intervertebral discs, the rubbery cushions between the vertebrae of your spine. Each disk has a soft, jelly-like center (nucleus) encased in a tougher exterior (annulus).
-
A slipped disk, also called a herniated or ruptured disk, occurs when part of the soft center pushes through a tear in the outer layer.
-
This can irritate nearby nerves, causing pain, numbness, or weakness in the affected limb.
-
Some people may have a slipped disk without any symptoms.
Symptoms
-
Localized pain and tenderness, often on one side of the body
-
Radiating pain to the arms or legs
-
Pain that worsens at night or with certain movements
-
Pain that increases after standing, sitting, or walking short distances
-
Unexplained muscle weakness
-
Tingling, aching, or burning sensations in the affected area
Effects / Complications
-
Chronic pain if untreated
-
Nerve compression, leading to weakness, numbness, or tingling
-
Reduced mobility or difficulty performing daily activities
-
In severe cases, loss of bladder or bowel control (medical emergency)
-
Muscle atrophy over time due to nerve damage
Treatment
1. Conservative / Non-surgical
-
Rest and activity modification (avoid heavy lifting, prolonged sitting)
-
Physical therapy to strengthen back and core muscles
-
Pain relief medications: NSAIDs, acetaminophen, or muscle relaxants
-
Hot/cold therapy to reduce inflammation and pain
-
Epidural steroid injections for severe nerve inflammation
2. Surgical options (if conservative treatment fails or in emergencies)
-
Discectomy – removal of the herniated portion of the disk
-
Laminectomy – removal of part of the vertebra to relieve pressure
-
Spinal fusion – joining two or more vertebrae to stabilize the spine
3. Preventive measures
-
Maintain good posture while sitting, standing, and lifting
-
Strengthen core muscles to support the spine
-
Avoid smoking, as it reduces blood flow to spinal disks
-
Maintain a healthy weight to reduce spinal stress
spinal injury
Spinal Cord Injury (SCI)
Overview
A spinal cord injury is damage to any part of the spinal cord or the nerves at the end of the spinal canal (cauda equina).
-
SCI often results in permanent changes in strength, sensation, and other body functions below the level of injury.
-
Depending on the location and severity, the injury may affect both sides of the body.
-
Injuries can impact physical, emotional, and social well-being, especially if recent.
Symptoms
-
Pain, numbness, or a burning sensation
-
Inability to move the arms or legs (paralysis)
-
Loss of sensation (pressure, heat, cold)
-
Muscle spasms
-
Loss of bladder or bowel control
-
Difficulty breathing (if injury is in the upper spinal cord)
Effects / Complications
-
Paralysis (paraplegia or quadriplegia)
-
Loss of sensation below injury level
-
Respiratory problems for higher-level injuries
-
Bladder and bowel dysfunction
-
Muscle atrophy and spasticity
-
Increased risk of pressure sores and infections
-
Emotional and psychological impact, including anxiety and depression
-
Secondary health issues: blood clots, cardiovascular problems, chronic pain
Treatment
1. Immediate Care
-
Immobilization of the spine to prevent further damage
-
Anti-inflammatory medications (e.g., corticosteroids) to reduce spinal cord swelling
-
Surgery to remove bone fragments, herniated discs, or foreign objects
2. Rehabilitation
-
Physical therapy to maintain muscle strength and prevent atrophy
-
Occupational therapy to improve daily living activities
-
Speech or respiratory therapy if injury affects breathing or speech
3. Medications
-
Pain management (analgesics, nerve pain medications)
-
Muscle relaxants for spasticity
-
Medications to support bladder and bowel function
4. Assistive Devices
-
Wheelchairs, braces, or walking aids
-
Adaptive devices for home and work environments
5. Psychological Support
-
Counseling and support groups for emotional well-being
-
Strategies to manage stress, anxiety, and depression
6. Long-Term Care
-
Prevent complications such as infections, pressure sores, and cardiovascular issues
-
Regular monitoring of bone density and overall health

Wrist Pain
Wrist Pain
Overview
Wrist pain is a common condition that can arise from multiple causes. The wrist is a complex structure composed of multiple small joints where the bones of the hand meet the forearm. It is essential for many daily activities, such as texting, writing, and lifting objects.
Wrist pain can result from:
-
Injuries (sprains, fractures, dislocations)
-
Repetitive strain (typing, sports, manual labor)
-
Arthritis or joint disorders
-
Inflammation of tendons or ligaments
A sudden injury, like a fall or twist, can overstretch ligaments, leading to acute pain, swelling, and limited movement. Chronic overuse may also cause long-term discomfort.
Symptoms
Signs of wrist pain may include:
-
Swelling
-
Warmth or heat over the joint
-
Pain (sharp or dull)
-
Discoloration (bruising)
-
Limited range of motion
-
Deformity (in severe cases)
Treatment / Management
-
Rest and immobilization: Use a splint or brace to reduce movement and allow healing.
-
Ice or cold therapy: Helps reduce swelling and inflammation.
-
Compression: Elastic bandages can help control swelling.
-
Elevation: Keep the wrist elevated above heart level to reduce swelling.
-
Medications: Pain relievers or anti-inflammatory drugs.
-
Physical therapy: Exercises to restore strength, flexibility, and function.
-
Surgery: Required in severe injuries (e.g., fractures, ligament tears) or persistent pain unresponsive to conservative care.
-
