Frostbite
Overview
Frostbite
Frostbite is an injury caused by freeze of the skin and underlying tissues. First your skin becomes terribly cold and red, then numb, hard and pale.
Frostbite is commonest on the fingers, toes, nose, ears, cheeks and chin. Exposed skin in cold, windy weather is most at risk of frostbite. But frostbite will occur on skin lined by gloves or different article of clothing.
Frostnip could be a milder type of cold injury that does not cause permanent skin harm. You can treat frostnip with first-aid measures, as well as rewarming the affected skin.
All different frostbite needs medical attention as a result of it will harm skin, tissues, muscle and bones. Possible complications of severe frostbite embody infection and nerve harm.
Symptoms
- Stages of frostbite
- Frostnip
- Signs and symptoms of frostbite include:
- At first, cold skin and a prickling feeling
- Numbness
- Red, white, bluish-white or grayish-yellow skin
- Hard or waxy-looking skin
- Clumsiness due to joint and muscle stiffness
Blistering after rewarming, in severe cases

Heat Rash
Heat Rash (Prickly Heat)
Overview
Heat rash, also known as prickly heat or miliaria, is not just a condition of babies—it can affect adults too, especially in hot and humid weather.
It develops when sweat ducts become blocked, trapping sweat beneath the skin.
Symptoms
-
Rash may feel prickly, burning, or intensely itchy.
-
Usually clears on its own once the skin is cooled.
-
Severe cases may require medical attention.
-
Adults often develop rash in skin folds or areas where clothing causes friction.
-
In infants, rash is common on the neck, shoulders, and chest, but can also appear in the armpits, elbow creases, and groin.
The best way to prevent and manage heat rash is by keeping the skin cool, dry, and avoiding excessive sweating.

Fissure and Fistula
Overview of Fissure and Fistula
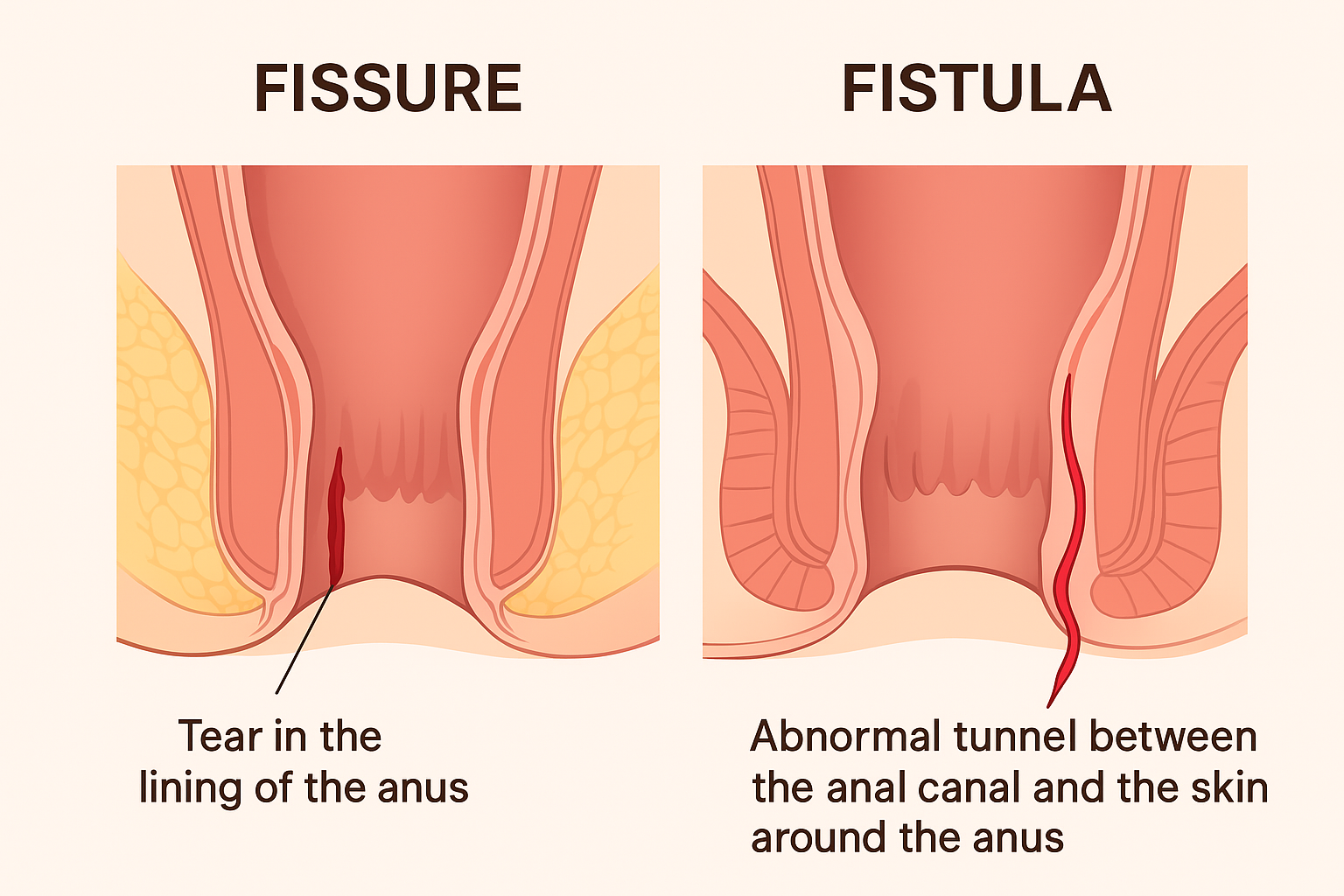
Anal Fissure
-
Definition:
A fissure is a small tear or crack in the lining of the anus. -
Causes:
-
Passing hard stools (constipation)
-
Straining during bowel movements
-
Chronic diarrhea
-
Childbirth trauma
-
-
Symptoms:
-
Severe pain during and after passing stool
-
Bright red blood on stool or tissue paper
-
Burning sensation and itching around the anus
-
Fear of passing stool due to pain
-
-
Complications:
-
Chronic fissures (if not treated)
-
Development of skin tags around anus
-
Anal Fistula
-
Definition:
A fistula is an abnormal tunnel that forms between the anal canal and the skin near the anus. -
Causes:
-
Most commonly due to anal abscess (infection with pus collection)
-
Chronic infections (e.g., Crohn’s disease, tuberculosis)
-
Trauma or surgery near anus
-
-
Symptoms:
-
Persistent pus or foul-smelling discharge near the anus
-
Pain and swelling around anal area
-
Recurrent abscess formation
-
Irritation and blood-stained discharge
-
-
Complications:
-
Chronic infection
-
Scarring and multiple fistula tracts
-
Recurrence if not properly treated
-
Key Difference
-
Fissure: A tear in the anal lining → causes pain and bleeding.
-
Fistula: A tunnel between anal canal and outer skin → causes pus discharge and infection.
Treatment Approach (Spaks Homeopathy)
-
Relieves pain, burning, discharge, and infection naturally.
-
Works on root causes like constipation, poor digestion, and weak tissues.
-
No side effects, no surgery, permanent solution possible.
Hyper Pigmentation
Overview
Hyperpigmentation occurs when the skin produces excess melanin, the natural pigment that gives skin its color. This leads to dark spots or patches that appear darker than the surrounding skin.
It is a very common skin condition that can affect people of all skin tones. Certain types, such as melasma, age spots, and sun spots, are more likely to appear on areas frequently exposed to the sun, such as the face, arms, and legs.
Symptoms
-
Brown, tan, or black spots on sun-exposed skin
-
Large darkened patches, often on the face or body
-
Uneven skin tone
-
Spots may become more noticeable after sun exposure
Effects
-
Cosmetic concern and reduced confidence due to uneven skin appearance
-
In some cases, may signal underlying conditions such as hormonal changes or post-inflammatory responses (after acne, injuries, or burns)
-
Without protection, patches may darken further with sun exposure
Treatment
1. Medical & Dermatological Treatments
-
Topical creams: Hydroquinone, retinoids, azelaic acid, kojic acid
-
Chemical peels: To lighten superficial pigmentation
-
Laser therapy: For stubborn or deep pigmentation
-
Microdermabrasion: To improve skin tone gradually
2. Home Care & Prevention
-
Always use sunscreen (SPF 30 or higher) daily
-
Avoid direct sun exposure, especially between 10 a.m. and 4 p.m.
-
Use protective clothing, hats, and sunglasses outdoors
-
Maintain a gentle skincare routine; avoid harsh scrubbing
3. Homeopathic Supportive Remedies (under professional advice)
-
Sepia – for brown patches, especially melasma
-
Sulphur – for uneven pigmentation with itching or dryness
-
Thuja occidentalis – for dark spots after skin eruptions or warts
-
Kali carbonicum – for pigmentation in women, especially during or after pregnancy
Key Point: Hyperpigmentation is usually harmless but can affect self-confidence. With proper sun protection, skincare, and medical treatment, dark patches can be reduced and managed effectively.

Hyperhidrosis
Overview
Hyperhidrosis (also called sudorrhea) is a condition characterized by excessive sweating beyond what the body needs for temperature regulation.
-
Sweating may affect a specific area (localized hyperhidrosis), such as the palms, soles, underarms, or face.
-
It may also affect the entire body (generalized hyperhidrosis).
-
Sweating often occurs in unusual situations, such as cool weather, or without any clear trigger.
-
In some cases, it may be caused by an underlying medical condition (secondary hyperhidrosis), such as diabetes, thyroid disorders, infections, or certain medications.
Symptoms
-
Excessive sweating in localized areas (hands, feet, armpits, face).
-
Clothing frequently soaked with sweat.
-
Sweating that interferes with daily activities.
-
Skin becoming soft, white, or peeling due to constant moisture.
-
Increased risk of skin infections.
-
Emotional distress, embarrassment, and social anxiety.
Effects of Hyperhidrosis
If untreated, hyperhidrosis can cause:
-
Skin irritation and infections (fungal or bacterial).
-
Difficulty handling objects (slippery hands).
-
Problems with writing, gripping, or using electronics.
-
Body odor due to bacterial growth.
-
Reduced confidence, anxiety, or depression.
Treatment Options
Medical Treatments
-
Antiperspirants (aluminum chloride-based) – first-line treatment for mild cases.
-
Prescription creams or oral medicines – reduce sweat production.
-
Iontophoresis – a device that passes mild electrical currents through skin to block sweat glands.
-
Botulinum toxin (Botox) injections – temporarily block nerve signals that trigger sweating.
-
Microwave therapy (miraDry) – destroys sweat glands in underarms.
-
Surgery (sympathectomy) – last resort, where certain nerves are cut to stop excessive sweating.
Home & Lifestyle Tips
-
Wear light, breathable clothing.
-
Use absorbent powders or sweat pads.
-
Stay hydrated to replace lost fluids.
-
Manage stress and anxiety, which can trigger sweating.
Homeopathic Support (complementary, under guidance)
-
Silicea – for clammy hands and feet.
-
Calcarea carbonica – for excessive sweating of the scalp and upper body.
-
Mercurius solubilis – for offensive sweat with body odor.
-
Psorinum – for profuse sweating that worsens at night.

Itchy skin
Itchy Skin (Pruritus)
Overview
Itchy skin, or pruritus, is an irritating sensation that makes you want to scratch. It can be mild, short-lived, or severe and persistent, interfering with daily life. Dry skin is one of the most common causes, especially in older adults.
Itchy skin may look normal or show visible changes like redness, bumps, or rough patches. Repeated scratching often worsens the condition, leading to skin damage, bleeding, or infections.
Relief often requires a mix of self-care, medical treatment, and addressing the root cause.
Symptoms
-
Localized itching (small areas like arms/legs) or generalized itching (whole body)
-
Redness
-
Bumps, spots, or blisters
-
Dry, cracked skin
-
Thickened, leathery, or scaly skin from scratching
Effects
If untreated, itchy skin can lead to:
-
Sleep disturbances due to constant discomfort
-
Skin damage (cuts, bleeding, sores)
-
Secondary bacterial infections from scratching
-
Emotional distress, irritability, or anxiety
-
In chronic cases, permanent skin changes (thick, dark patches or scars)
Treatment
Self-care/Home Remedies:
-
Use fragrance-free moisturizers several times a day
-
Bathe with lukewarm water (avoid hot water)
-
Use gentle, non-soap cleansers
-
Apply cold compresses for relief
-
Keep nails short to reduce skin damage from scratching
Medical Treatments (depending on cause):
-
Medicated creams/ointments (corticosteroids, calcineurin inhibitors)
-
Antihistamines (for allergy-related itching)
-
Anti-itch lotions with menthol, camphor, or pramoxine
-
Phototherapy (light treatment for chronic itching)
-
Treatment of underlying conditions (eczema, psoriasis, liver/kidney issues, thyroid problems, etc.)

Keloids
Keloids
Overview
A keloid is a type of raised scar that develops when the skin heals after an injury. Unlike normal scars, keloids grow beyond the original wound area and may continue enlarging over time.
They can occur after:
-
Cuts, burns, or surgical wounds
-
Severe acne
-
Body piercings or tattoos
-
Vaccinations or even minor skin trauma
Keloids are not harmful or contagious, but they can be uncomfortable, itchy, or affect appearance. Some may stop growing after a few months, while others keep enlarging for years.
Symptoms of Keloids
Keloids often have the following features:
-
Slow growth: May appear 3 months to 1 year after skin injury and enlarge over weeks or months.
-
Raised and thick: A firm, elevated scar with a flat or shiny surface.
-
Color changes: Often start pink or red, then darken. They usually become darker than the person’s skin tone, with borders darker than the center.
-
Texture changes: Can feel soft and doughy, or hard and rubbery compared to surrounding skin.
-
Discomfort: May cause itching, pain, or tenderness while growing. Symptoms usually improve once growth stops.
Effects of Keloids
While keloids are not life-threatening, they can cause:
-
Cosmetic concerns (especially on visible areas like the face, neck, or chest)
-
Itching and irritation
-
Restricted movement if they form near joints (shoulders, elbows, knees)
-
Emotional or social distress due to appearance
Treatment Options
Keloids can be difficult to treat, and no single method works for everyone. Treatments aim to flatten, shrink, or reduce symptoms:
-
Corticosteroid injections: Reduce inflammation and flatten scars.
-
Cryotherapy (freezing): Shrinks smaller keloids.
-
Laser therapy: Helps flatten and lighten scars.
-
Surgery: Removes the keloid, but recurrence is common unless combined with other treatments.
-
Silicone sheets or gels: Applied over the scar to soften and flatten it.
-
Radiation therapy or pressure dressings: Sometimes used after surgery to lower recurrence risk.
-
Home remedies: Moisturizing creams, avoiding irritation, and protecting from sun exposure may help reduce discomfort.

Keratosis
Overview
Keratosis pilaris
Keratosis pilaris may be a common, harmless skin condition that causes dry, rough patches and little bumps, typically on the higher arms, thighs, cheeks or buttocks.
The bumps generally don't hurt or itch. Keratosis pilaris is usually thought-about a variant of normal skin.
It can't be cured or prevented. But you'll be able to treat it with moisturizers and prescription creams to assist improve the looks of the skin. The condition usually disappears by age 30.
Symptoms
- Close-up of keratosis pilaris
- Keratosis pilaris will occur at any age, however it's a lot of common in young kids.
- Signs and symptoms include:
- Painless little bumps, usually on the higher arms, thighs, cheeks or buttocks
- Dry, rough skin in the areas with bumps
- Worsening once seasonal changes cause low wetness and skin tends to be drier
- Sandpaper-like bumps resembling goose flesh
