Leprosy
Leprosy (Hansen’s Disease)
Overview
Leprosy, also known as Hansen’s disease, is a chronic bacterial infection caused by Mycobacterium leprae. It mainly affects the skin, nerves, mucous membranes, and eyes. Contrary to common belief, leprosy is not highly contagious. Transmission is thought to occur through droplets from the nose or mouth of untreated patients after prolonged, close contact.
Around 95% of people are naturally immune, which means only a small portion of those exposed will develop the disease. With early diagnosis and treatment, leprosy is curable, and disability can be prevented.
Symptoms
-
Light-colored or reddish skin patches that persist for weeks or months
-
Skin patches with reduced sensation (touch, pain, heat)
-
Numbness in hands, feet, arms, and legs (“glove and stocking anesthesia”)
-
Muscle weakness and paralysis (leading to deformities of hands/feet)
-
Eye problems (can lead to blindness if untreated)
-
Enlarged nerves, especially around the elbows and knees
-
Stuffy nose and nosebleeds
-
Ulcers on soles of the feet
-
Curling of fingers and thumb due to paralysis of small hand muscles
Effects
If untreated, leprosy can cause:
-
Permanent nerve damage
-
Disfigurement of hands, feet, and face
-
Blindness due to eye involvement
-
Chronic ulcers and secondary infections
-
Social stigma and psychological distress
Treatment
Leprosy is completely curable with appropriate medication:
-
Multidrug therapy (MDT) is the standard treatment, using a combination of antibiotics (dapsone, rifampicin, and clofazimine). Treatment duration ranges from 6 months to 2 years, depending on severity.
-
Anti-inflammatory drugs (such as corticosteroids) may be used to manage nerve pain and inflammation.
-
Surgery or physiotherapy may be required to correct deformities or restore function.
-
Self-care: Regular skin and wound care to prevent infections and complications.
Prevention & Care
-
Early detection and treatment prevent transmission.
-
Close contacts of leprosy patients may receive preventive therapy.
-
Education and awareness help reduce stigma.

Moles
Moles (Nevi)
Overview
Moles are one of the most common types of skin growths. They usually appear as small, dark brown spots caused by clusters of pigment-producing cells called melanocytes.
Moles often develop during childhood or adolescence, and most people have between 10 and 40 moles. Some may change in appearance or fade with age.
While most moles are harmless, in rare cases, they may develop into skin cancer (melanoma). This makes regular monitoring of moles and other pigmented skin patches very important.
Symptoms / Characteristics
-
Color & Texture – Moles may be brown, tan, black, red, blue, or pink. They can be smooth, wrinkled, flat, or raised. Some may have hair growth.
-
Shape – Most moles are oval or round.
-
Size – Usually smaller than 1/4 inch (6 mm) in diameter (about the size of a pencil eraser).
-
Congenital Moles (present at birth) – May be larger and cover wider areas of the skin, such as the face, limbs, or body.
Effects / Risks
-
Cosmetic concern – Visible moles may affect appearance.
-
Irritation – Moles in high-friction areas (waistline, armpits, neck) may get irritated.
-
Cancer risk (Melanoma) – Rarely, moles may turn into cancer. Warning signs include:
-
Rapid growth or enlargement
-
Irregular/blurred borders
-
Uneven or multiple colors
-
Bleeding, itching, or pain
-
Change in shape, size, or texture
-
Treatment & Management
Medical Care
-
Observation – Most moles require no treatment, just monitoring.
-
Surgical removal – A dermatologist may remove moles that are suspicious, irritating, or unwanted cosmetically.
-
Biopsy – If a mole looks abnormal, a small tissue sample may be tested to rule out cancer.
Self-Care & Prevention
-
Protect skin with broad-spectrum sunscreen (SPF 30 or higher).
-
Avoid tanning beds and prolonged sun exposure.
-
Perform monthly self-checks of skin.
-
Use the ABCDE rule (Asymmetry, Border, Color, Diameter, Evolution) to spot unusual moles.
-
Visit a dermatologist annually or whenever a mole changes.
Homeopathic Support (for harmless moles, under guidance)
-
Thuja Occidentalis – for small skin growths and warts.
-
Sulphur – for rough, itchy skin with multiple moles.
-
Calcarea Carbonica – for individuals prone to multiple skin spots.
-
Nitric Acid – for painful or sensitive moles.

Perioral Dermatitis
Perioral Dermatitis
Overview
Perioral dermatitis is an inflammatory skin condition that affects the area around the mouth. When the rash spreads to the nose, eyes, or other facial areas, it is also referred to as periorificial dermatitis.
The rash typically appears as red, scaly, or bumpy skin and may be accompanied by fluid-filled lesions, mild itchiness, or burning sensations. While the condition is more common in women aged 16–45, it can occur in all ages, races, and children.
Without appropriate treatment, perioral dermatitis may subside temporarily but often recurs, and individual episodes can last for weeks to months.
Symptoms
-
Rash of red bumps around the mouth and in the folds of the nose
-
Scaly or rough texture of the affected skin
-
Rash may also appear:
-
Under the eyes
-
On the forehead
-
On the chin
-
-
Mild itching, burning, or stinging sensations
-
Occasionally, clear fluid discharge from bumps
Effects
-
Cosmetic concern and reduced self-confidence due to visible facial rash
-
Chronic or recurring episodes may cause emotional stress or frustration
-
Persistent inflammation can increase sensitivity of the facial skin
-
Overuse of topical steroids may worsen the condition (steroid-induced perioral dermatitis)
Treatment
Treatment focuses on reducing inflammation, controlling infection, and preventing recurrence:
1. Discontinuing Triggers:
-
Stop using topical corticosteroids, heavy facial creams, or irritating skincare products
-
Avoid fluoridated toothpaste if it worsens the rash
2. Medications:
-
Topical antibiotics (e.g., metronidazole or clindamycin)
-
Oral antibiotics for more severe or widespread cases (e.g., doxycycline or tetracycline)
3. Skin Care Recommendations:
-
Use gentle, non-irritating cleansers
-
Avoid harsh scrubbing or exfoliation
-
Moisturize with light, non-comedogenic products
4. Lifestyle Measures:
-
Avoid excessive sun exposure or wear broad-spectrum sunscreen
-
Manage stress, which may trigger flare-ups
-
Follow up with a dermatologist for recurrent or severe cases

Piles
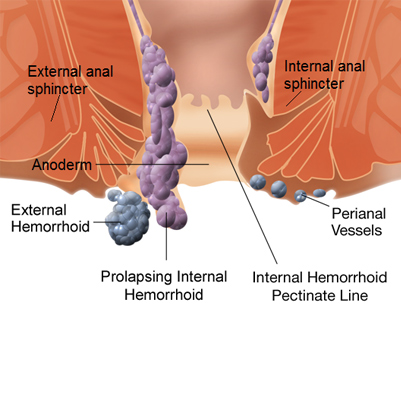
What are Piles?
Piles, also known as Hemorrhoids, is a condition in which the veins around the anus become swollen.
These swollen veins appear like lumps or warts, and may cause –
Pain
Itching
Burning sensation
And sometimes bleeding
In mild cases, piles can be treated with home remedies and medicines.
But if the problem keeps recurring or becomes severe, proper medical treatment is necessary.
Types of Piles
Internal Piles:
These are located 2–4 cm above the anal opening. This is the most common type.
External Piles:
These occur on the outer edge of the anus and can be easily seen or felt.
Symptoms of Piles
-
Hard and painful lump around the anus
-
Feeling of incomplete bowel movement even after passing stool
-
Fresh red blood during or after bowel movement
-
Itching and burning around the anus
-
Pain while passing stool
When Can It Become Serious?
If left untreated, piles can lead to:
-
Continuous bleeding and anemia
-
Infection
-
Fecal incontinence (inability to control bowel movements)
-
Anal fistula (an abnormal channel between the anal canal and the skin near the anus)
-
Strangulated hemorrhoid (when blood supply to the hemorrhoid is cut off, causing clot or infection)
Treatment of Piles at Spaks Homeopathy
At Spaks Homeopathy, piles, fissure, and fistula can be treated effectively with homeopathy.
The best part is –
Permanent cure is possible
No side effects
No surgery required
Spaks Homeopathy’s special medicines, creams, and oils help in quickly reducing pain, burning, and bleeding, and provide long-term relief by treating the root cause.
Ringworm
Ringworm of the Body (Tinea Corporis)
Overview
Ringworm of the body is a fungal infection that develops on the outermost layer of the skin. Despite the name, no worms are involved.
-
It is characterized by a red, circular rash with clearer skin in the center.
-
Also related to other fungal infections such as:
-
Athlete’s foot (tinea pedis)
-
Jock itch (tinea cruris)
-
Ringworm of the scalp (tinea capitis)
-
Transmission:
-
Direct skin-to-skin contact with an infected person or animal
-
Contact with contaminated objects such as clothes, towels, or bedding
Most cases respond well to topical antifungal medications, but oral antifungal pills may be needed for extensive or resistant infections.
Symptoms
-
Flat, scaly patches that may be red and itchy
-
A raised border that expands outward, forming a circular or ring-like shape
-
The inner area may be clear, scaly, or have scattered red bumps
-
Multiple rings can develop and overlap
-
Sometimes mild burning or irritation
Effects / Complications
-
Persistent itching and discomfort
-
Skin cracking or secondary bacterial infection due to scratching
-
Spread to other parts of the body if untreated
-
Contagion to family members or close contacts
-
Cosmetic concerns due to visible rashes
Treatment
-
Topical Antifungal Medications (for mild cases)
-
Clotrimazole, miconazole, terbinafine creams applied once or twice daily for 2–4 weeks
-
Keep affected area clean and dry
-
-
Oral Antifungal Medications (for severe or widespread cases)
-
Terbinafine, itraconazole, or fluconazole as prescribed by a doctor
-
Usually taken for 2–6 weeks, depending on severity
-
-
Self-care / Home Measures
-
Wash hands thoroughly after touching infected areas
-
Avoid sharing towels, clothes, or bedding
-
Wear loose, breathable clothing to reduce moisture
-
Clean and disinfect contaminated surfaces and objects
-
-
Prevention
-
Maintain good personal hygiene
-
Treat pets if they are infected
-
Avoid direct contact with infected individuals or contaminated objects
-

Shingles
Shingles (Herpes Zoster)
Overview
Shingles is a viral infection caused by the varicella-zoster virus, the same virus that causes chickenpox. After chickenpox resolves, the virus remains dormant in nerve tissues near the spinal cord and brain. Years later, it may reactivate as shingles.
-
Typically affects one stripe of skin on one side of the body, most often the torso.
-
Shingles is not usually life-threatening but can be very painful.
-
Vaccination can reduce the risk, and early treatment can shorten the duration and prevent complications.
Symptoms
-
Pain, burning, numbness, or tingling in a localized area
-
Sensitivity to touch
-
Red rash appearing a few days after the pain begins
-
Fluid-filled blisters that break open and form crusts
-
Itching in the affected area
Effects / Complications
-
Postherpetic neuralgia: Persistent nerve pain after the rash heals
-
Vision or hearing problems if shingles affects the eyes or ears
-
Skin infections from scratching or blister rupture
-
Neurological issues in rare cases (e.g., facial paralysis, encephalitis)
-
Emotional distress due to chronic pain
Treatment
1. Medical / Antiviral Therapy
-
Antiviral medications (acyclovir, valacyclovir, famciclovir) to reduce viral activity
-
Pain management with analgesics, NSAIDs, or stronger pain medications if needed
-
Corticosteroids in some cases to reduce inflammation
2. Symptom Relief / Supportive Care
-
Cool compresses to soothe the rash and blisters
-
Calamine lotion or colloidal oatmeal baths for itching
-
Keeping the rash clean and dry to prevent secondary infections
3. Prevention
-
Shingles vaccine recommended for older adults (50+) or those at high risk
-
Maintaining a healthy immune system through proper diet, sleep, and stress management

Skin Infection
Skin Infection
Overview
The skin is the largest organ of the body, serving as a protective barrier against infection, injury, and environmental hazards.
A skin infection occurs when bacteria, viruses, fungi, or parasites penetrate the skin and begin to multiply, causing inflammation and damage.
-
Causes:
-
Bacteria: Staphylococcus aureus, Streptococcus species (can cause cellulitis, impetigo, boils)
-
Fungi: Dermatophytes, Candida (can cause ringworm, athlete’s foot, candidiasis)
-
Viruses: Herpes simplex, varicella-zoster (can cause cold sores or shingles)
-
Parasites: Scabies mites, lice
-
-
Infections can range from mild (treatable at home) to severe (requiring medical intervention).
Symptoms
Mild skin infections:
-
Redness or rash
-
Itching
-
Small bumps, pimples, or pustules
-
Pain or tenderness
Severe skin infections:
-
Pus or fluid-filled blisters
-
Skin sloughing or breakdown
-
Darkened or discolored skin
-
Painful areas with intense itching
-
Fever or malaise if the infection spreads
Effects / Complications
-
Local tissue damage and scarring
-
Spread of infection to other areas of the skin or deeper tissues
-
Sepsis or bloodstream infection in severe bacterial infections
-
Chronic skin conditions if untreated (e.g., recurrent fungal infections)
Treatment
-
Mild infections
-
Clean the affected area with mild soap and water
-
Apply over-the-counter antibiotic or antifungal creams
-
Keep the area dry and protected
-
Avoid scratching or picking at lesions
-
-
Moderate to severe infections
-
Prescription topical or oral antibiotics/antifungals/antivirals
-
Drainage of abscesses or boils if necessary
-
Hospitalization for severe cases with systemic symptoms
-
-
Preventive measures
-
Maintain good hygiene
-
Avoid sharing personal items (towels, razors)
-
Keep cuts and scrapes clean and covered
-
Wear protective clothing in high-risk environments
-

Sunburn
Sunburn
Overview
Sunburn is red, painful skin that feels hot to the touch, usually appearing hours after excessive exposure to ultraviolet (UV) light from sunlight or artificial sources like sunlamps.
Repeated or intense sun exposure increases the risk of:
-
Premature skin aging: Wrinkles, dark spots, and rough skin
-
Skin cancers: Including basal cell carcinoma, squamous cell carcinoma, and melanoma
-
Long-term skin damage
Most sunburns heal in a few days, but severe burns may require medical attention. Preventive care and skin protection are essential, even on cloudy days.
Symptoms
Sunburn can vary in severity. Common symptoms include:
-
Pinkness or redness of the skin
-
Skin that feels hot or warm to the touch
-
Pain, tenderness, or itching
-
Swelling
-
Small fluid-filled blisters that may break
-
Headache, fever, nausea, and fatigue (in severe cases)
Effects / Complications
-
Pain and discomfort lasting several days
-
Skin peeling or blistering
-
Dehydration in severe sunburns
-
Increased risk of skin infections if blisters break
-
Long-term risk of skin cancer and premature aging
Treatment / Management
1. Immediate Care
-
Move out of the sun and rest in a cool place
-
Apply cold compresses or take cool baths to reduce heat
-
Avoid popping blisters to prevent infection
2. Moisturizing & Skin Care
-
Use aloe vera gel or fragrance-free moisturizers
-
Apply soothing lotions with calamine or hydrocortisone cream for pain and inflammation
3. Pain & Inflammation Relief
-
Over-the-counter pain relievers like ibuprofen or acetaminophen
-
Hydration: Drink plenty of water to prevent dehydration
4. Prevention
-
Apply broad-spectrum sunscreen (SPF 30 or higher)
-
Wear protective clothing, hats, and sunglasses
-
Limit sun exposure, especially during peak UV hours (10 a.m.–4 p.m.)
-
Reapply sunscreen every 2–3 hours and after swimming or sweating
